The healthcare industry is pouring billions into artificial intelligence with the goal of revolutionizing patient care, yet the digital messages patients receive often feel more like automated spam than genuine support. This disconnect lies at the heart of a growing problem where technology designed to connect is instead creating distance. Despite booming investments, a recent analysis reveals that patient engagement tools are significantly underperforming, leaving both patients and providers frustrated.
This isn’t just a technological hiccup; it’s a critical failure with human and financial costs. A study of over 75 U.S. health system executives found that a staggering 95% are unsatisfied with their current tools for addressing common issues like medication adherence and missed appointments. These gaps in engagement contribute directly to poor health outcomes and add billions in avoidable costs to the healthcare system annually, raising the urgent question of why these well-funded solutions are falling so flat.
The Trillion Dollar Paradox of Patient Engagement
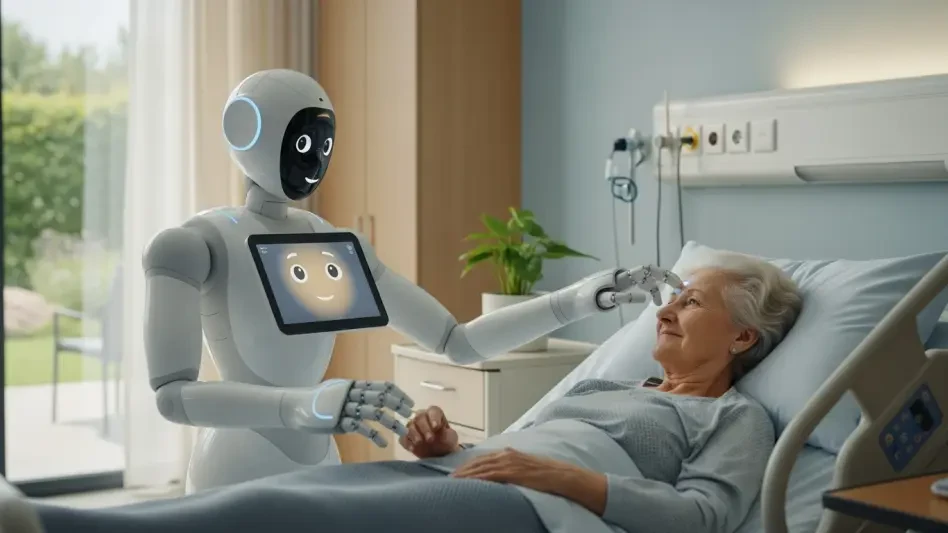
The vision for AI in healthcare was one of profound personalization. The technology promised to serve as a supportive digital partner for every patient, offering guidance and encouragement tailored to their unique health journey. This idealized future saw AI not as a cold, automated system but as an extension of compassionate care, available 24/7 to help individuals navigate their health needs with confidence.
However, the current reality is a stark contrast to that initial promise. For many patients, interactions with healthcare AI are generic, unhelpful, and ultimately alienating. The common experience of receiving a robotic appointment reminder or a one-size-fits-all health tip often leads to disengagement rather than empowerment. These communications lack the empathy and understanding that form the foundation of a trusted patient-provider relationship, feeling less like care and more like a poorly targeted advertisement.
Deconstructing a Flawed Definition of Personalization
The core of the problem lies in how current systems define “personalization.” Most AI platforms operate on a superficial level, using basic demographic data to create the illusion of a tailored experience. Personalization often begins and ends with inserting a patient’s first name into a template or segmenting audiences by broad categories like age or gender. This approach treats individuals as data points rather than complex human beings.
This surface-level segmentation fails because it ignores the crucial “why” behind a patient’s behavior. Consider the generic mammogram reminder sent to all women over 40. Such a message cannot distinguish between a patient who simply forgot and one who is avoiding the appointment due to deep-seated anxiety, a lack of childcare, or inflexible work hours. Without understanding these individual barriers, the AI’s attempt at personalization is not only ineffective but can also feel tone-deaf and impersonal.
An Expert Diagnosis Mistaking Data for Connection
According to Amy Bucher, Chief Behavioral Officer at Lirio, the industry is fundamentally mistaking data aggregation for genuine human connection. Bucher argues that true personalization requires moving beyond broad demographic buckets to understand the specific motivations, beliefs, and barriers of each individual. It is about comprehending the nuanced psychology that drives a person’s health decisions, not just their statistical profile.
Clinicians excel at this type of empathetic, one-on-one interaction during appointments, but it is impossible for them to apply that same level of individualized attention across thousands of patients. This is precisely the gap that technology was meant to fill. Yet, current AI strategies have failed to replicate this human-centric approach, instead doubling down on data-driven models that lack the sophisticated understanding needed to foster a real connection and inspire action.
Prescribing a New Model N of 1 Personalization
A more effective solution is emerging in the form of an “N-of-1” personalization model. This framework represents a paradigm shift, moving away from segmenting populations to treating each patient as a unique, individual case. It is designed to understand and communicate with one person at a time, creating a truly bespoke experience that resonates on a personal level.
This advanced model leverages agentic AI and reinforcement learning to process complex datasets far beyond simple demographics. It analyzes behavioral patterns, communication preferences, and psychosocial factors to generate messaging tailored to a single person’s specific circumstances. For instance, for the one in ten Americans with diabetes who may be disengaged from their care, this approach can deliver outreach that addresses their specific hurdles, whether it is cost, transportation, or motivation, thereby sparking renewed interest and action.
The implementation of this N-of-1 model showed that it could drive tangible results. By communicating with patients in a way that acknowledged their unique situations, health systems saw measurable clinical improvements and created significant operational efficiencies. This shift demonstrated that the future of patient engagement depended not on more data, but on smarter, more empathetic technology that finally learned to treat each patient as the individual they are.