Introduction to a Healthcare Revolution
In the remote upazilas of Bangladesh, millions of rural residents face a harsh reality: access to basic medical care is often a distant dream, with only 7 doctors available per 10,000 people compared to the World Health Organization’s recommended 23. This staggering disparity paints a grim picture of healthcare in developing nations, where systemic shortages of professionals and infrastructure leave communities vulnerable to preventable illnesses. Artificial Intelligence (AI) emerges as a beacon of hope, offering innovative solutions to bridge these gaps by empowering local health workers and extending specialist-level diagnostics to the farthest corners. This analysis delves into the pressing challenges of rural healthcare, explores AI’s growing role as a transformative force, incorporates expert insights, and envisions future possibilities, culminating in a compelling call for collaborative action to ensure equitable health access.
The Current Landscape of Rural Healthcare Challenges
Persistent Disparities and Structural Barriers
Rural healthcare in Bangladesh stands at a critical juncture, burdened by a severe lack of resources. Data from recent health surveys reveal that the majority of medical professionals are concentrated in urban centers, leaving rural areas with minimal access to trained personnel. The World Health Organization highlights that this imbalance results in overcrowded district hospitals, where patients often endure inhumane conditions due to bed shortages.
Beyond numbers, systemic issues compound the crisis. Long travel distances to reach medical facilities deter many from seeking timely care, while reliance on untrained “village doctors” remains a risky norm for isolated communities. These structural deficiencies create a cycle of neglect that disproportionately affects the most vulnerable populations in regions like remote upazilas.
Tangible Consequences of Limited Access
The real-world impact of these healthcare gaps is devastating, as delayed treatments for manageable conditions lead to unnecessary suffering. Consider Salma Begum, a fictional community health worker in a rural village, who struggles daily to provide care with limited training and resources, often watching preventable illnesses escalate due to the absence of local expertise. Her story mirrors countless others across Bangladesh.
Specific areas, such as Cox’s Bazar with its refugee-heavy population, face even greater strain on already fragile systems. Here, the lack of immediate medical intervention often turns minor ailments into life-threatening emergencies, underscoring the urgent need for innovative solutions to support rural caregivers and patients alike.
AI as a Game-Changer for Rural Healthcare
Rising Technologies and Adoption Trends
AI is rapidly gaining traction as a vital tool in healthcare, particularly in low-resource settings. Global trends show increasing adoption in countries like Thailand and India, where digital health solutions are transforming remote care delivery. Reports indicate significant investments in health tech, with scalable AI tools demonstrating high accuracy in diagnostics, even in underserved regions.
Specific innovations, such as AI-driven analysis of chest X-rays for tuberculosis detection and portable ultrasound devices integrated with smartphones, are proving revolutionary. Studies suggest these tools achieve near-specialist precision, offering immense potential for widespread impact in rural areas of developing nations like Bangladesh, where such technology can redefine access.
Real-World Applications and Promising Outcomes
Concrete examples illustrate AI’s transformative power in rural settings. Smartphone apps for symptom triage enable health workers to prioritize urgent cases, while initiatives like Google’s diabetic retinopathy screening through retinal imaging address chronic conditions without the need for on-site specialists. These tools are already making a difference globally.
In Bangladesh, the introduction of portable AI-ultrasound devices marks a historic step, empowering midwives and health workers to diagnose complications on the spot. Such advancements provide real-time guidance, as seen in remote clinics where community caregivers now deliver improved outcomes, reducing the strain on distant hospitals and fostering trust among villagers.
Expert Perspectives on AI’s Role in Rural Healthcare
Insights from Leaders in Health and Technology
Global health experts and technologists view AI as a critical ally in narrowing rural healthcare gaps. Many emphasize its capacity to act as a force multiplier, extending limited medical resources to underserved areas. A paraphrased opinion from a WHO representative stresses that AI can enhance diagnostic reach, provided it is tailored to local needs.
However, challenges like data bias and inadequate infrastructure are frequently cited concerns. Experts warn that algorithms trained on non-representative datasets may falter in rural contexts, necessitating robust local data collection. Policymakers in Bangladesh also highlight the importance of integrating AI without undermining the essential human element in patient care.
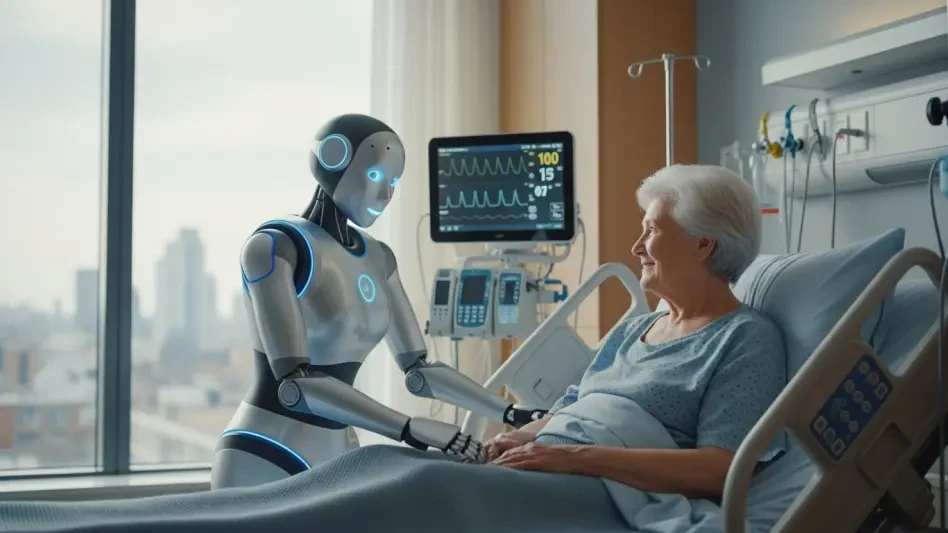
Balancing Innovation with Human Connection
A strong consensus exists on the need for a human-technology synergy in healthcare delivery. AI should support, not replace, the personal touch that rural communities value in their caregivers. This balance ensures that tools empower health workers to make informed decisions while maintaining trust and empathy at the core of medical interactions.
Future Outlook for AI in Rural Healthcare
Envisioning a Tech-Enabled Healthcare System
Looking ahead, equipping Bangladesh’s 18,000 community clinics with AI-powered diagnostic kits holds immense promise. Localized software in Bangla could further enhance usability, enabling health workers to deliver precise care directly in villages. Such advancements might significantly reduce hospital burdens over the coming years.
Potential benefits include better health outcomes for millions, as early detection and intervention become standard even in remote areas. Yet, challenges persist, including unreliable internet connectivity and high initial costs, which could hinder equitable rollout if not addressed through strategic planning and investment.
Broader Implications and Necessary Safeguards
The broader impact of AI in rural healthcare hinges on developing localized models that reflect regional disease patterns and cultural nuances. Public-private partnerships and supportive government policies are essential to ensure access for the poorest communities, preventing technology from widening existing disparities.
Privacy risks associated with digitized health records also loom large, demanding stringent safeguards. Without careful oversight, there’s a danger that AI solutions might remain out of reach for marginalized groups, underscoring the need for inclusive frameworks that prioritize equity in deployment and access.
Reflecting on a Path Forward
Looking back on the exploration of AI’s role in rural healthcare, it is evident that the dire state of access in areas like Bangladesh has created an urgent need for innovation. The transformative potential of AI stands out as a powerful means to empower community health workers and bring specialist care to remote regions. Expert cautions have highlighted the importance of addressing data biases and infrastructure limitations to ensure effectiveness.
Moving forward, stakeholders—governments, technology firms, and health organizations—must prioritize collaborative efforts to develop sustainable, localized AI solutions. Investing in rural connectivity, training programs, and privacy protections emerges as critical next steps to guarantee that technology serves as a tool for equity. The journey ahead demands a commitment to integrating human compassion with digital progress, ensuring that no community is left behind in the quest for better health outcomes.