The global health crisis of the early 2020s inadvertently launched a revolution not in a laboratory or a hospital, but on the kitchen tables and bathroom counters of millions of ordinary people. This mass adoption of self-assessment tools, from rapid antigen tests to at-home diagnostics for urinary tract infections and colon cancer, shattered long-held assumptions about the public’s role in managing health. It proved that individuals can reliably collect critical health data, setting a powerful precedent for the next, more profound evolution in patient care: structured self-treatment. This shift from passive recipient to active participant is no longer a futuristic concept but an urgent necessity, driven by a healthcare system buckling under the weight of its own inefficiencies.
When the Waiting Room Becomes the Biggest Barrier to Wellness
For countless individuals, the primary obstacle to receiving care is not the complexity of their condition but the logistical nightmare of accessing a clinician. Protracted waiting periods for appointments have become the norm, forcing patients to delay treatment for days or even weeks. This systemic delay is compounded by the practical burdens of travel, securing transportation, and taking unpaid time off from work—barriers that turn a simple check-up into a significant personal and financial challenge.
These hurdles are magnified for those in rural or low-resource communities, where the nearest clinic can be hours away. The friction involved in seeking professional care often leads to avoidance, allowing manageable health issues to fester. A minor infection or a slow-healing wound, left unchecked due to these access gaps, can escalate into a severe, life-threatening complication, transforming a preventable problem into a medical crisis that strains both the patient and the healthcare system.
The Breaking Point of a System Under Strain
The strain on the healthcare system is not merely a patient-facing issue; it is an internal crisis reaching a critical tipping point. The traditional doctor-centric model has created an unsustainable bottleneck, placing an impossible demand on clinicians. They are tasked with seeing an ever-increasing volume of patients while navigating immense administrative burdens and data management, a combination that has fueled an epidemic of professional burnout. This exhaustion of the clinical workforce directly compromises the quality and availability of care for everyone.
This fragile infrastructure is fundamentally ill-equipped to handle the rising tide of chronic diseases. With conditions like diabetes affecting over 38 million Americans, the demand for continuous, long-term management far outstrips the capacity of a system built for episodic, in-person consultations. The current model simply cannot scale to meet this challenge, creating a care deficit that leaves millions of patients without the consistent support needed to manage their health effectively.
A New Paradigm for Patient Empowerment
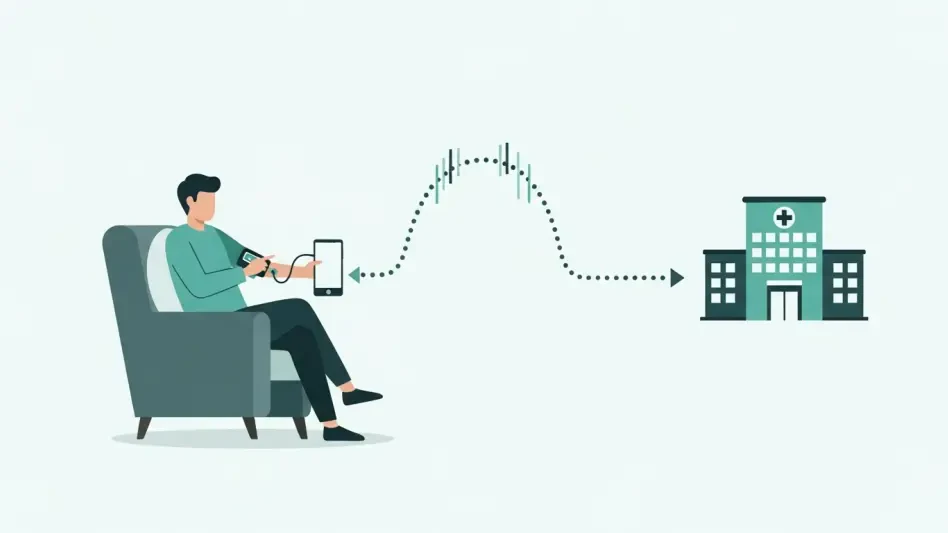
In response to this systemic crisis, a new model of structured self-treatment is emerging, one that must be carefully distinguished from unsupervised “DIY medicine.” This is not about abandoning patients to figure things out alone. Instead, it involves empowering them with affordable, user-friendly tools, clear digital guidance, and structured protocols to execute prescribed care plans safely from their own homes, all under the remote supervision of their clinical team.
This approach represents a logical and powerful extension of recent healthcare innovations. Just as telehealth, remote patient monitoring, and hospital-at-home programs have decentralized care, structured self-treatment further extends the reach of clinical expertise. The core principle is not to replace clinicians but to scale their guidance, allowing one expert’s care plan to support numerous patients simultaneously. The clinician remains central to diagnosis and oversight, but the execution of routine, repetitive treatment tasks becomes a shared, empowered responsibility.
The Ripple Effect of At-Home Healing
Conditions requiring consistent, ongoing management, such as diabetes and chronic wound care, serve as ideal proving grounds for this model. A patient with a diabetic foot ulcer, for instance, can be equipped to clean and redress the wound at home by following interactive digital instructions, while their care team remotely monitors photos and data to track healing progress. This method not only grants patients greater autonomy but also has a profound impact on health equity, removing the logistical barriers that often prevent vulnerable populations from receiving timely care and avoiding dire outcomes like amputation.
The economic and systemic benefits are equally compelling. In the United States, chronic wounds alone incur an estimated annual cost of $50 billion. Preventing just a single wound-related hospitalization, which can easily exceed $30,000, generates substantial savings for payers. Moreover, by shifting routine care into the home, this model unlocks critical capacity within clinics and hospitals. It allows overburdened healthcare professionals to redirect their finite time and expertise toward the most complex and acute cases, enhancing overall system efficiency and mitigating the burnout crisis.
Forging a Path to Safe and Equitable Self-Care
The successful widespread adoption of self-treatment hinges on a robust framework built on three pillars: safety, training, and equity. It is not enough to simply provide the tools; patients must receive comprehensive training on how to apply treatments correctly and, critically, how to recognize early warning signs that necessitate professional intervention. Clear protocols and easy access to clinical support are essential to ensure that patient empowerment does not lead to unintended harm.
Furthermore, this new paradigm must be implemented equitably to avoid deepening existing health disparities. The necessary tools, technologies, and digital guidance must be affordable and accessible to all, regardless of income, location, or technical literacy. Seamless integration with professional care networks is paramount, ensuring that data from at-home treatments flows directly to clinicians for oversight. Encouragingly, much of the foundational infrastructure, including insurance coverage for many necessary products, is already in place to support this transition.
This evolution ultimately reimagined the role of the patient and the definition of a clinical setting. It proposed a system where homes became active centers for healing and individuals were transformed into engaged partners in their own wellness journey. The successful integration of structured self-treatment demonstrated a path toward a more sustainable, equitable, and effective healthcare future, built not on adding more bricks to overburdened hospitals, but on empowering millions in the very place they call home.