Today, we’re thrilled to sit down with Faisal Zain, a renowned expert in healthcare technology with a deep background in the manufacturing of medical devices for diagnostics and treatment. Faisal has been at the forefront of driving innovation in this space, and his insights into how artificial intelligence is transforming large-scale health systems are invaluable. In this conversation, we’ll explore the strategic integration of AI in healthcare, focusing on governance frameworks, the importance of reducing inconsistencies in care, the role of frontline staff in technology adoption, and the balance between AI augmentation and human decision-making. We’ll also dive into practical applications like staffing solutions and documentation improvements, shedding light on how AI is enhancing patient safety and operational efficiency.
How did you first become interested in the intersection of AI and healthcare technology, and what excites you most about its potential?
My journey into AI and healthcare technology started with a fascination for how data could solve real-world problems in medicine. Early in my career, while working on diagnostic devices, I saw firsthand how much variability existed in patient outcomes due to inconsistent processes. AI, with its ability to analyze massive datasets and uncover patterns, struck me as a game-changer. What excites me most today is its potential to not just improve efficiency but to save lives by catching issues early, personalizing treatments, and reducing errors. It’s about making healthcare more equitable and accessible, which feels like a mission worth pursuing every day.
Can you walk us through the importance of a strong governance structure when implementing AI in a large healthcare system?
Absolutely. Governance is the backbone of any successful AI integration, especially in a complex environment like healthcare where stakes are incredibly high. A robust structure ensures that AI initiatives align with patient safety, ethical standards, and organizational goals. It’s not just about having clinical leaders at the table; you need input from operations, finance, IT, and even legal teams to assess risks and opportunities from every angle. This diversity of perspectives helps prioritize projects based on impact and feasibility while ensuring no department feels sidelined. Without this, you risk deploying tools that don’t address real needs or, worse, create unintended harm.
What does reducing variance in clinical and operational areas mean to you, and why is it a priority for AI applications?
Reducing variance is about minimizing inconsistencies in how care is delivered or how operations are managed. In clinical settings, this could mean ensuring that patients with similar conditions receive the same standard of care regardless of their location or the clinician’s experience level. Operationally, it might involve streamlining processes like supply chain management. AI excels at identifying where these discrepancies occur and providing data-driven solutions to standardize outcomes. This directly translates to better patient safety and more predictable, efficient workflows for staff. It’s a priority because consistency is often the difference between good and great care.
Why do you believe involving frontline staff early in the AI deployment process is so critical?
Frontline staff—nurses, doctors, and support teams—are the ones who interact with patients and systems daily. They know the pain points better than anyone sitting in a boardroom. Bringing them into the process early ensures that AI tools address actual problems rather than theoretical ones. Their feedback can reveal practical challenges, like usability issues or workflow disruptions, that might not be obvious otherwise. More importantly, involving them builds trust and buy-in, which is essential for adoption. If they feel heard, they’re more likely to champion the technology rather than resist it.
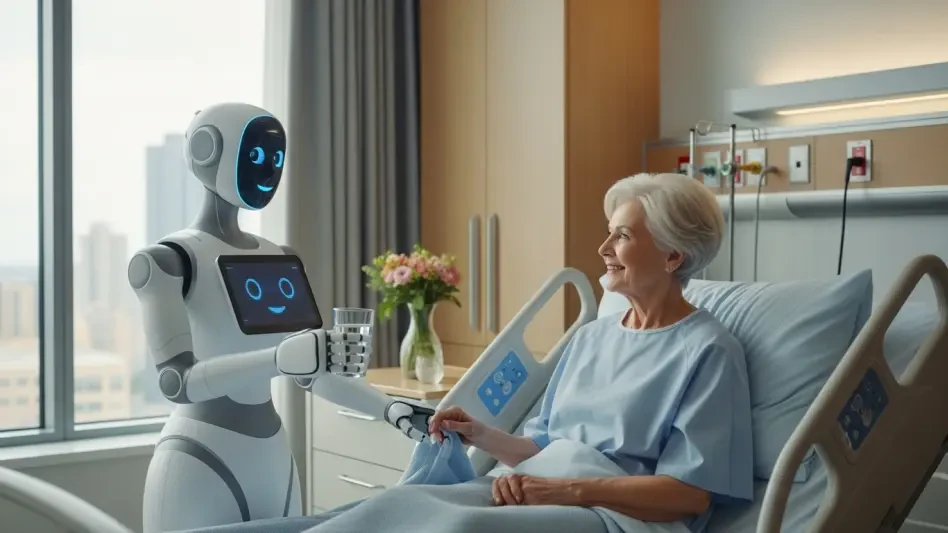
How do you see AI augmenting human decision-making in healthcare, as opposed to fully automating it?
AI augmentation is about empowering clinicians, not replacing them. In a clinical setting, this might mean providing doctors with real-time data insights during a diagnosis—like flagging potential issues in a patient’s chart based on historical trends—while leaving the final call to the physician. It’s different from automation, which might handle repetitive tasks like scheduling without human input. The key is to design AI as a supportive tool that enhances judgment, preserves the human touch in care, and respects the nuanced decisions that only experienced professionals can make. Some areas, like interpreting emotional cues from patients, should always remain human-driven.
Can you share how AI is transforming something as practical as staffing in healthcare settings?
Staffing is a perfect example of where AI can make a huge difference. Before AI, scheduling nurses or other staff often relied on manual processes that took hours and didn’t always account for patient needs or staff expertise. AI can analyze variables like patient acuity, staff availability, and skill sets to create balanced schedules dynamically. For instance, it ensures a mix of experienced and newer nurses on a shift to match the complexity of cases on a unit. The impact is significant—staff spend less time on administrative headaches, workloads are better distributed, and patient care improves because the right people are in the right place at the right time.
What role does AI play in easing the burden of documentation for healthcare providers?
Documentation has long been a source of frustration for clinicians, often pulling them away from patient interaction to spend hours at a computer. AI, particularly ambient technology, is changing that by allowing providers to dictate notes naturally during patient encounters. The system captures the conversation, understands context, and organizes it into the electronic health record accurately. This not only saves time but also creates more complete records, which improve communication between shifts and support better decision-making. Ultimately, it gives clinicians more time at the bedside, which boosts both their job satisfaction and patient experience.
What is your forecast for the future of AI in healthcare over the next decade?
I believe the next decade will see AI become even more seamlessly integrated into healthcare, moving beyond specific tools to a holistic part of care delivery. We’ll likely see advancements in predictive analytics, where AI anticipates patient deterioration or outbreaks before they happen, enabling proactive interventions. Personalization of treatments will also grow, with AI tailoring therapies based on genetic and lifestyle data. However, the biggest shift will be in accessibility—AI could help bridge gaps in underserved areas through telemedicine and remote diagnostics. The challenge will be ensuring equity and maintaining trust, but if we get the balance right, AI has the potential to redefine what quality healthcare looks like globally.