Today, we’re diving into the transformative world of healthcare technology with Faisal Zain, a renowned expert in medical technology. With a deep background in the manufacturing of diagnostic and treatment devices, Faisal has been at the forefront of driving innovation in the industry. In this conversation, we explore how artificial intelligence is reshaping the doctor-patient relationship, the potential for technology to humanize care, the risks and ethical concerns surrounding AI, and the challenges of ensuring equitable access to these advancements.
How has the dynamic between doctors and patients evolved over the years, and what’s driving the tension we see today?
Over the years, the doctor-patient relationship has undergone a significant shift, largely due to the increasing pressures of the healthcare system. The core issue is what I call the “business of medicine.” Doctors are often pushed to see more patients in shorter time slots to meet financial or administrative demands. This rush diminishes the ability to build trust and truly connect with patients, which is at the heart of quality care. It’s a systemic challenge that leaves both doctors and patients feeling frustrated.
What impact does this time crunch have on the quality of medical care?
When doctors are forced to prioritize quantity over quality, it inevitably affects the care they provide. There’s less time to listen to a patient’s concerns, delve into their medical history, or explain complex diagnoses. This can lead to miscommunication, missed details, or even errors. Ultimately, it erodes the personal touch that’s so vital in medicine, leaving patients feeling like they’re just another number on a chart.
In what ways can artificial intelligence step in to improve the healthcare experience?
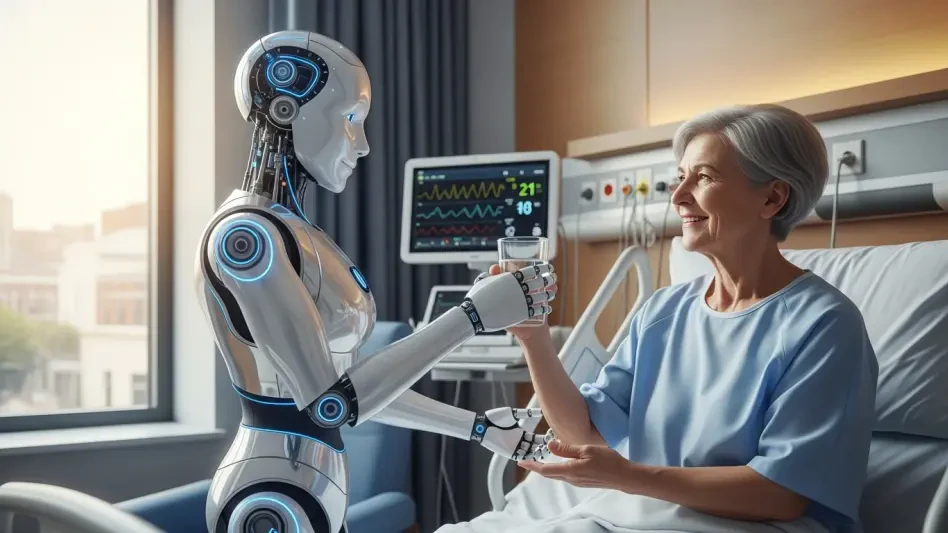
AI has incredible potential to alleviate some of these pressures. By automating time-consuming tasks like administrative paperwork, data entry, and even preliminary diagnostics, AI can free up doctors to focus on what matters most—interacting with their patients. It’s about giving back that precious time so doctors can listen, empathize, and provide thoughtful care, rather than being bogged down by clerical work.
How can AI make medical interactions feel more personal rather than mechanical?
It might sound counterintuitive, but technology like AI can actually bring a human touch back to medicine. For instance, AI tools can analyze vast amounts of patient data to provide tailored insights or predict potential health issues. When a doctor shares these personalized insights with a patient—maybe showing them a visual breakdown of their health risks—it fosters a deeper understanding and connection. It turns a routine visit into a meaningful conversation.
Can you share a specific example of how AI is already supporting healthcare providers or patients?
Absolutely. One exciting application is in predictive analytics. I’ve seen systems where doctors input patient data into AI-driven databases that compare it against millions of other cases. The result is a detailed report on potential health risks specific to that individual. This not only helps doctors make informed recommendations but also empowers patients by giving them a clearer picture of their health. It’s already transforming how care is delivered in many clinics.
What concerns do you have about how the time saved by AI might be utilized?
I do worry that the time AI frees up could be misused if the focus shifts purely to efficiency or profit. There’s a risk that healthcare systems might push doctors to see even more patients rather than using that time to enhance care quality. We need strong guidelines to ensure that this gift of time benefits patients directly, preserving the sanctity of the doctor-patient bond over business interests.
How can we ensure AI prioritizes patient well-being over the financial goals of healthcare organizations?
It starts with advocacy and policy. We need to involve patients, doctors, and ethicists in shaping how AI is implemented, ensuring the focus remains on improving outcomes rather than just cutting costs. Transparency is key—healthcare providers should be open about how AI is used and demonstrate that it’s enhancing care. Additionally, regulations can help hold organizations accountable to prioritize patient needs over bottom lines.
What are some of the biases present in healthcare, and how do they manifest in AI systems?
Bias in healthcare is a reflection of broader societal inequities, and it often shows up in disparities in treatment or access based on race, gender, or socioeconomic status. When AI systems are trained on historical data, they can inadvertently perpetuate these biases. For example, if past data underrepresents certain demographics, the AI might not accurately predict or address their health needs. It’s a significant challenge that requires deliberate effort to correct.
Could AI help reduce these biases, or does it risk amplifying them further?
AI has the potential to do both, depending on how it’s designed and deployed. If we consciously address bias by using diverse datasets and involving underrepresented communities in development, AI can help level the playing field by identifying and correcting disparities in care. However, if we’re not careful, it can worsen existing inequities by reinforcing flawed patterns. It’s all about intentional design and continuous monitoring.
What challenges do you see in ensuring equal access to AI technologies in healthcare?
Unequal access is a major hurdle. Advanced AI tools often roll out first in well-funded hospitals or affluent areas, leaving underserved communities behind. This digital divide means that those who need these innovations most—often low-income or rural populations—miss out. Bridging this gap requires investment in infrastructure, training, and policies that prioritize equitable distribution of technology across all regions and demographics.
Beyond access, what other barriers might prevent AI from benefiting all patients?
There are several other obstacles. For one, there’s a lack of trust in AI among both patients and providers, often due to skepticism about its accuracy or ethical implications. Then there’s the issue of integration—many healthcare systems aren’t equipped to adopt new tech seamlessly due to outdated systems or insufficient training. Lastly, cultural or language barriers can hinder effective use of AI tools if they’re not designed with diverse populations in mind.
Despite these challenges, what keeps you optimistic about AI’s role in the future of medicine?
I’m optimistic because of the sheer scale of problems AI can help solve. Take diagnostic errors, for instance—we see millions of serious mistakes each year, and AI has the potential to significantly reduce that number by providing second opinions or flagging inconsistencies. Beyond that, I believe AI will improve patient outcomes in the near future by enabling earlier interventions and more precise treatments. The challenges are real, but the promise of better, more compassionate care drives my hope.
What is your forecast for the role of AI in healthcare over the next decade?
I foresee AI becoming an integral part of healthcare, not as a replacement for doctors but as a powerful partner. In the next ten years, I expect AI to streamline workflows even further, enhance personalized medicine through advanced data analysis, and play a key role in addressing global health disparities if we tackle access issues. It’s an exciting time, but it will require collaboration across sectors to ensure AI serves humanity first and foremost.