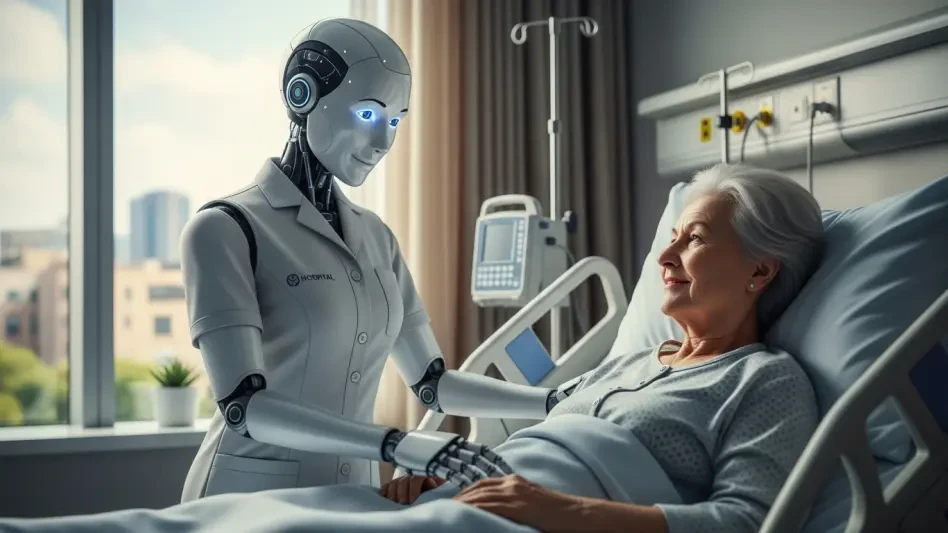
I’m thrilled to sit down with Faisal Zain, a trailblazer in healthcare technology with a deep background in medical device manufacturing for diagnostics and treatment. With years of experience driving innovation, Faisal has been at the forefront of integrating cutting-edge solutions like artificial intelligence into clinical practice. In our conversation, we explore how AI is reshaping decision-making, enhancing patient care, and streamlining workflows, while also diving into the challenges of adoption, the importance of transparency, and the future of multidisciplinary teamwork in healthcare.
How did your journey in healthcare technology begin, and what drew you to focus on AI as a transformative tool?
My career started in the manufacturing of medical devices, where I saw firsthand how technology could bridge gaps in diagnostics and treatment. I was always fascinated by the potential of tools to improve accuracy and efficiency. As AI emerged as a game-changer, I realized it could do more than just support—it could augment clinical judgment in ways we hadn’t seen before. My passion for innovation and better patient outcomes naturally led me to explore how AI could be seamlessly woven into healthcare workflows.
What changes have you observed in the perception of technology in healthcare over the years?
When I started, technology was often seen as a luxury rather than a necessity in healthcare. There was skepticism due to concerns about safety, data privacy, and regulatory hurdles. Back then, even basic digital tools were patchy and not fully integrated. Over time, with advancements in secure data handling and compliance frameworks, those barriers have lessened. Now, there’s a growing acceptance that technology, especially AI, can be a vital partner in decision-making, provided it’s designed with clinician input and focused on real needs like time-saving and better outcomes.
Can you share a memorable instance where AI directly influenced a patient’s outcome in a clinical setting?
Absolutely. I recall a challenging case involving an elderly patient with a complex medical history, including a leg infection and kidney issues. Manually sorting through potential treatments and drug interactions would’ve taken ages. Using an AI tool, we input the patient’s details and received evidence-based recommendations in seconds—covering everything from monitoring to potential risks. It not only saved time but also ensured a safer, clearer plan for the patient. That moment reinforced how AI can act as a powerful ally in urgent care scenarios.
In what ways has AI altered the time clinicians can dedicate to building relationships with patients?
AI has been a game-changer in freeing up precious minutes during consultations. Tasks like note-taking or pulling together fragmented data, which used to eat into face-to-face time, are now handled swiftly with tools like speech recognition or automated documentation. Saving even a few minutes per patient means clinicians can focus on meaningful interactions—explaining conditions, reassuring patients, or providing resources. This directly boosts trust and improves how patients engage with their care.
What resistance have you encountered from peers when introducing AI into healthcare settings, and how do you tackle it?
Resistance often stems from fears that AI might replace clinicians or from distrust in so-called ‘black box’ systems where the reasoning isn’t clear. I address this by emphasizing that AI is assistive, not autonomous—it’s only as good as the input and the human judgment guiding it. I also advocate for transparency, pushing for tools designed as ‘glass boxes’ where clinicians can see the logic, sources, and limitations behind suggestions. Sharing success stories and involving peers in tool development helps turn skepticism into curiosity and eventual adoption.
How do you approach explaining AI-driven recommendations to patients to maintain their confidence in your care?
I treat AI as a reference tool that enhances, not dictates, my decisions. I often use it in real-time during consultations, showing patients the evidence it pulls up. For instance, with a patient weighing treatment options, I queried an AI tool to compare risks and benefits, then walked them through the data while clarifying that I’m still the one making the final call. This transparency reassures them that we’re using validated insights, not guesswork, and it strengthens their trust in the process.
How do you see AI shaping collaboration within multidisciplinary healthcare teams?
AI has incredible potential to streamline communication across specialties in multidisciplinary teams. Imagine a case where a cardiologist, oncologist, and nurse are collaborating—AI can summarize relevant evidence tailored to each perspective, cutting down on miscommunication and delays. I’ve seen trials where AI provided faster, referenced reasoning for decisions in critical care, even aiding in justifying steps like insurance approvals. It reduces friction, speeds up consensus, and ensures everyone has access to the same insights, regardless of their specialty.
What is your forecast for the role of AI in healthcare over the next decade?
I believe AI will become an indispensable part of healthcare, evolving from a novel tool to a standard component of clinical workflows. We’ll see deeper integration into areas like personalized medicine, predictive analytics, and even training the next generation of clinicians. The focus will shift toward making AI more intuitive and clinician-friendly, ensuring it addresses real pain points while maintaining strict ethical and safety standards. If we foster collaboration between tech developers and healthcare providers, I’m confident AI will help us tackle global challenges like workforce shortages and access to care, ultimately transforming how we deliver health services.