The labyrinthine process of prior authorization, a persistent source of administrative friction and delays in patient care, is now at the center of a technological revolution driven by artificial intelligence. The adoption of AI represents a significant advancement in the healthcare administration sector, promising to untangle this complexity. This review will explore the evolution of AI methodologies, their key features, performance capabilities, and the impact they have on the prior authorization process. The purpose of this review is to provide a thorough understanding of these technologies, their current applications, and their potential for future development in ensuring efficiency, compliance, and clinical integrity.
The Emergence of AI in Utilization Management
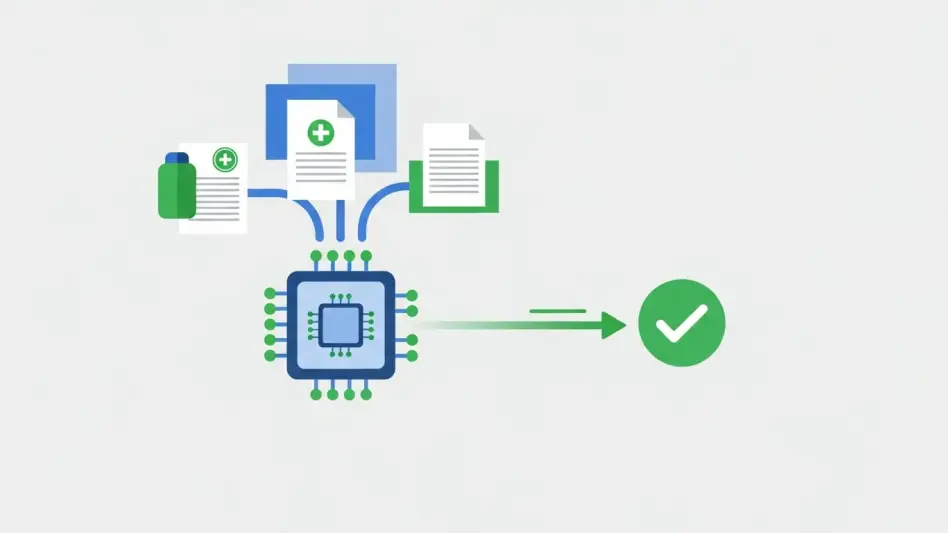
The integration of artificial intelligence into utilization management marks a pivotal shift from manual, labor-intensive processes toward automated, data-driven workflows. Historically, prior authorization has been a bottleneck, characterized by cumbersome paperwork and lengthy review cycles that strain provider resources and delay patient access to care. AI emerged as a solution to this challenge, offering the capacity to process vast amounts of clinical data against complex policy rules at a scale and speed unattainable by human reviewers alone.
At its core, AI in this context involves using algorithms to analyze clinical information submitted by providers and compare it to payers’ medical policies to determine if a requested service or treatment is medically necessary. This application is not a monolithic technology but rather a spectrum of methodologies, each with distinct strengths and weaknesses. Its relevance is magnified by an increasingly complex healthcare environment, where administrative burdens and intricate regulatory requirements demand more sophisticated tools for maintaining both operational efficiency and clinical oversight.
A Comparative Analysis of AI Methodologies
Analytical AI for Compliance and Precision
Analytical AI stands as a foundational component for modern prior authorization systems, operating on deterministic, rule-based logic. This methodology processes structured data by applying a predefined set of rules derived directly from clinical guidelines and payer-specific medical policies. Its primary strength lies in its predictability and consistency; for a given set of inputs, the output is always the same. This deterministic nature makes it exceptionally well-suited for high-stakes environments where every decision must be justifiable and aligned with established standards.
The performance of analytical AI is measured by its precision and its capacity for auditability. Because each step of its decision-making process follows a clear, codified pathway, the rationale behind an automated approval can be traced and verified. This transparency is not merely a technical benefit but a crucial requirement for adhering to strict regulatory frameworks. For payers and providers, this means that automated determinations are defensible, transparent, and built on a foundation of clinical evidence, ensuring that technology enhances, rather than replaces, the principles of sound medical judgment.
Generative AI for Supportive Non-Decisional Tasks
In contrast, generative AI functions by creating new content based on patterns learned from immense datasets. Technically, models like large language models (LLMs) operate probabilistically, generating outputs that are statistically likely but not guaranteed to be factually accurate or logically consistent. This makes generative AI a powerful tool for administrative support roles, such as summarizing extensive clinical notes for a human reviewer, drafting patient communications, or streamlining documentation workflows. In these tasks, its ability to synthesize information and produce human-like text can significantly reduce administrative overhead.
However, these same characteristics render generative AI unsuitable for core decision-making in prior authorization. Its probabilistic nature means it can produce variable or even fabricated information—often referred to as “hallucinations”—and its internal logic is opaque, making its conclusions inherently unauditable. Applying such a model to determine medical necessity would introduce an unacceptable level of risk, potentially leading to inconsistent denials, compliance violations, and an erosion of trust between payers and providers. Its role, therefore, must be confined to supportive tasks that do not require deterministic, policy-adherent outcomes.
Predictive AI for Proactive Healthcare Planning
Predictive AI occupies a different niche, focusing on using historical data to forecast future events and identify trends. In a clinical context, predictive models can analyze patient data to identify individuals at high risk for developing chronic conditions or to anticipate hospital readmissions, enabling proactive interventions. Within utilization management, this technology can help optimize resource allocation by forecasting demand for specific services. Its function is to provide insights that support strategic planning and population health management.
While powerful, predictive AI is an advisory tool, not a decisional one. Its forecasts are based on correlations and probabilities, not on the specific clinical evidence for an individual case. As a result, its outputs are intended to inform human judgment rather than replace it. For prior authorization, a prediction that a patient group is likely to need a certain therapy is valuable for network planning, but the final determination of medical necessity for any individual patient must still be based on a direct evaluation of their clinical data against established policies, a task for which analytical AI is better suited.
The Evolving Regulatory and Compliance Landscape
The trajectory of AI in prior authorization is being shaped significantly by an evolving regulatory environment. In recent years, there has been intensifying scrutiny from federal and state regulators on the use of automated systems, particularly concerning “AI denials.” Health plans are facing increasing pressure to ensure their decision-making processes are transparent, explainable, and clinically sound. This movement is driven by concerns that opaque algorithms could lead to inappropriate denials of care without clear, reviewable justification.
This trend is solidified by new federal mandates, most notably the CMS Interoperability and Prior Authorization Final Rule. Set to take effect in 2027, this rule imposes stringent requirements on payers, including the mandate to provide specific reasons for all denials and to streamline communication between payers and providers through standardized APIs. These regulations place a premium on accountability and traceability, creating a landscape where AI solutions must be fully auditable. This regulatory push inherently favors technologies like analytical AI, which can provide a clear, step-by-step rationale for every automated determination.
Real-World Implementation of Analytical AI
In a practical setting, the implementation of analytical AI transforms the prior authorization workflow from a reactive, manual process into a proactive, intelligent one. The core of this model involves embedding policy-aligned intelligence directly into the electronic health record (EHR) or payer portal. This system works by codifying a health plan’s specific medical policies and clinical guidelines into a set of deterministic rules. When a provider submits a request, the system evaluates the structured clinical data against these codified policies in real time.
This technology is designed specifically to automate approvals when the submitted data clearly meets the established criteria for medical necessity. If the information aligns perfectly with policy, the request is approved instantly, reducing turnaround times from days to seconds. Critically, if the case presents any ambiguity, complexity, or does not meet the clear criteria for approval, the system does not issue a denial. Instead, it automatically flags the request and routes it to a licensed clinician for manual review. This “human-in-the-loop” approach ensures that AI is used to augment clinical expertise, not to circumvent it, thereby maintaining clinical integrity while gaining administrative efficiency.
Addressing the Challenges and Risks of AI Adoption
Despite its promise, the adoption of AI in prior authorization is not without significant challenges and risks. The primary concern revolves around applying inappropriate AI models to a process that demands absolute precision and compliance. Using probabilistic models like generative or predictive AI for core decision-making introduces risks of inconsistency, bias, and a lack of transparency, which can lead to regulatory penalties and compromised patient care. The technical challenge lies in ensuring that the chosen AI can interpret complex clinical data accurately and apply nuanced policy logic consistently.
To mitigate these limitations, ongoing development efforts are focused on creating systems that are inherently transparent and auditable. The most responsible approach involves designing AI frameworks that keep clinicians firmly in control of complex decisions. This involves building clear escalation pathways for cases that fall outside the scope of automation and providing tools that give human reviewers full insight into the data and logic the AI used. The goal is not to achieve full automation but to create a symbiotic relationship where technology handles routine, clear-cut approvals, freeing up clinical experts to focus their attention on the complex cases that require their judgment.
Future Outlook and Strategic Considerations for Payers
Looking ahead, the evolution of AI in healthcare administration will continue to focus on deeper integration and greater intelligence. Future developments will likely involve enhancing the ability of analytical AI to process more varied forms of clinical data while maintaining its deterministic core. The push for interoperability will also drive the creation of more seamless systems that can share data and decisions across the healthcare ecosystem, further reducing friction in processes like prior authorization.
For payers navigating this landscape, selecting the right AI solution requires a strategic and discerning approach. It is crucial to move beyond marketing buzzwords and ask pointed questions about how a system functions. Key considerations should include whether the technology uses the payer’s specific medical policies as its foundation or relies on less reliable historical data patterns. Payers must demand to see how each decision is made and verify that the system is designed to defer to clinicians whenever a case requires expert review. The ultimate measure of a successful AI implementation will be its ability to deliver efficiency without sacrificing transparency, compliance, or clinical oversight.
Conclusion: Adopting the Right AI for Responsible Innovation
The review of AI methodologies in prior authorization has illuminated a clear distinction between different approaches and their suitability for this critical healthcare function. The analysis confirmed that while various forms of AI offer value, their application must be carefully matched to the task at hand. Generative and predictive AI, though powerful in supportive and planning capacities, were found to lack the necessary transparency and deterministic logic required for making auditable medical necessity determinations.
Ultimately, the evidence pointed toward analytical AI as the most appropriate and responsible choice for automating core prior authorization decisions. Its rule-based, deterministic framework aligns directly with the stringent demands for compliance, auditability, and clinical integrity that govern utilization management. By automating clear approvals while ensuring complex cases are deferred to human experts, analytical AI presented a model for innovation that enhances efficiency without compromising patient safety or regulatory adherence. This balanced approach represented the most effective path forward for payers seeking to modernize their operations responsibly.