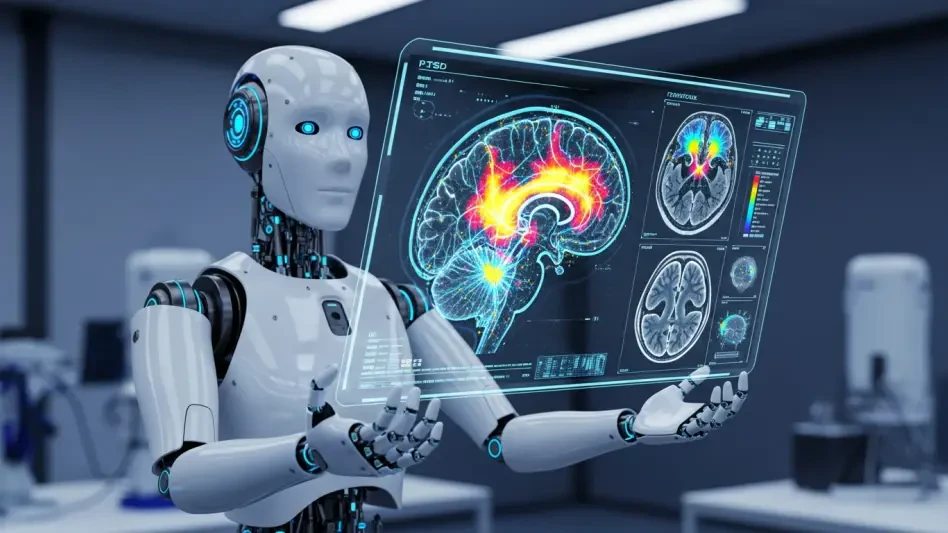
In a world where mental health challenges often remain hidden beneath the surface, consider that millions of individuals suffering from Post-Traumatic Stress Disorder (PTSD) have historically faced misdiagnosis or dismissal due to the invisible nature of their condition, underscoring a critical gap in healthcare. This staggering reality highlights the inability to objectively identify and treat trauma-related disorders with precision. Today, a groundbreaking convergence of artificial intelligence (AI) and advanced neuroimaging technologies is poised to change this landscape, offering hope for accurate diagnosis and tailored care. This industry report delves into how these innovations are revolutionizing PTSD management, reshaping mental health practices, and addressing long-standing societal stigmas. By exploring technical advancements, clinical impacts, market dynamics, and future prospects, this analysis aims to illuminate a transformative era in precision psychiatry.
Revolutionizing Mental Health: The Intersection of AI and Neuroimaging
The mental health sector stands at a pivotal moment, driven by rapid advancements in AI and neuroimaging that are redefining how PTSD and other invisible trauma conditions are understood and treated. Historically, diagnosing such disorders has been fraught with challenges due to their lack of visible symptoms, relying heavily on subjective patient reports and clinician observations. This often led to inconsistent outcomes and delayed interventions, leaving many without proper care. The integration of cutting-edge tools like functional MRI (fMRI), structural MRI (sMRI), Positron Emission Tomography (PET), Electroencephalography (EEG), and Magnetoencephalography (MEG), combined with AI models such as machine learning and deep learning, marks a significant shift toward data-driven, objective approaches.
This technological synergy is not merely an incremental improvement but a fundamental reorientation of mental healthcare. By leveraging AI to analyze complex brain imaging data, the industry is moving toward precision psychiatry, where treatments are customized to individual neurobiological profiles. The significance of this shift extends beyond clinical settings, promising to enhance global mental health outcomes by validating patient experiences with measurable evidence. As these tools uncover hidden patterns in brain activity and structure, they pave the way for early detection and personalized therapies, setting a new standard for trauma care.
Technological Innovations Driving PTSD Care
Cutting-Edge Neuroimaging Techniques
Advanced neuroimaging modalities are at the forefront of revealing the intricate brain alterations caused by trauma, providing insights that were previously unattainable. Techniques such as fMRI capture dynamic changes in brain activity through blood flow measurements, while Diffusion Tensor Imaging (DTI) assesses the integrity of white matter connections. PET scans offer a window into metabolic shifts, highlighting how trauma impacts energy use in critical areas like the hippocampus, amygdala, and prefrontal cortex, which are central to emotional regulation and memory.
These tools excel in detecting subtle damage that eludes traditional methods, such as microscopic changes from mild traumatic brain injury (TBI) or the lingering effects of childhood trauma. By mapping specific neural disruptions, neuroimaging enables clinicians to pinpoint the biological underpinnings of PTSD symptoms. This level of detail is crucial for developing targeted interventions that address the root causes rather than merely alleviating surface-level manifestations.
AI’s Analytical Power in Trauma Diagnosis
Complementing neuroimaging, AI brings unparalleled analytical capabilities to the table, transforming raw data into actionable insights for PTSD diagnosis. Algorithms like Support Vector Machines and Convolutional Neural Networks excel at processing high-dimensional imaging datasets, often achieving diagnostic accuracies exceeding 90% when integrated with multimodal inputs such as genetic and physiological markers. These systems identify biomarkers that signal trauma’s presence long before symptoms become severe.
Beyond detection, AI plays a vital role in predicting symptom progression and treatment responses, enabling proactive care strategies. Tools like Explainable AI further enhance clinical trust by making complex predictions interpretable, ensuring that healthcare providers can understand and act on AI-driven recommendations. This analytical prowess not only streamlines diagnosis but also lays the groundwork for identifying novel therapeutic targets, pushing the boundaries of trauma management.
Clinical and Societal Impacts of AI-Driven PTSD Care
From Subjective to Objective Diagnostics
The transition from subjective assessments to objective diagnostics represents a seismic shift in PTSD care, addressing decades of diagnostic uncertainty. By identifying concrete biomarkers through neuroimaging and AI, clinicians can now validate the neurological basis of trauma with precision. This approach significantly reduces the risks of misdiagnosis and underdiagnosis, ensuring that patients receive timely and appropriate interventions.
Moreover, objective evidence of brain changes empowers healthcare providers to design personalized treatment plans tailored to each patient’s unique neurobiological profile. Early intervention becomes more feasible, preventing the escalation of symptoms and improving long-term outcomes. This shift also fosters greater patient trust in the medical system, as their experiences are substantiated by measurable data rather than dismissed as intangible.
Broader Societal Benefits and Challenges
The societal implications of these technologies extend far beyond individual care, promising to reshape public perceptions of mental health. Objective validation of invisible injuries combats stigma, encouraging more people to seek help without fear of judgment. This cultural change could lead to improved mental health outcomes on a global scale, particularly in communities where such conditions are often taboo or misunderstood.
However, significant challenges temper these benefits, including concerns over the privacy of sensitive brain data and the potential for algorithmic bias to exacerbate inequities in care. Ensuring equitable access to these advanced technologies remains a pressing issue, as high costs and limited infrastructure could exclude vulnerable populations. Addressing these hurdles is essential to maximize the societal impact of AI and neuroimaging in trauma care.
Corporate Dynamics and Market Opportunities
Key Players and Competitive Landscape
The market for AI and neuroimaging in mental health is bustling with activity, as diverse players from tech giants to startups drive innovation in PTSD diagnostics and care. Companies like Alphabet and IBM contribute robust computational infrastructure and ethical frameworks, facilitating the scaling of AI solutions. Their involvement ensures that data processing and storage meet the stringent demands of clinical applications.
Meanwhile, startups such as Icometrix and Cortechs.ai carve out specialized niches, focusing on areas like veteran care and TBI detection with FDA-approved tools. These smaller entities often lead in agility, bringing tailored algorithms to market swiftly. The competitive landscape is shaped by a shared goal of early detection and personalized care, with each player contributing unique strengths to address the multifaceted needs of trauma management.
Market Growth and Future Potential
The emerging market for AI and neuroimaging in mental health is poised for substantial growth, fueled by increasing demand for precise diagnostics and tailored treatments. Industry projections suggest significant expansion over the next few years, driven by access to diverse datasets and regulatory approvals that validate these technologies for clinical use. Performance indicators point to a rising adoption rate among healthcare providers seeking innovative solutions.
Key factors for market success include interdisciplinary talent that bridges technology and psychiatry, alongside continuous algorithmic advancements. Looking ahead, opportunities for disruption abound in diagnostics, treatment planning, and enhancing accessibility through scalable AI tools. This dynamic environment signals a fertile ground for investment and innovation, promising to reshape mental health delivery on a global scale.
Challenges and Barriers to Adoption
The integration of AI and neuroimaging into PTSD care faces a spectrum of technical, ethical, and logistical obstacles that could hinder widespread adoption. Data scarcity poses a significant barrier, as training robust AI models requires vast, diverse datasets that are often unavailable or inconsistent across populations. High costs associated with advanced imaging equipment further limit accessibility, particularly in under-resourced regions.
Ethical concerns also loom large, with the opacity of some AI models—often termed a “black box”—raising questions about clinical reliability and trust. Privacy risks tied to brain data collection demand stringent safeguards, while the potential for algorithmic bias threatens to perpetuate disparities in care. Addressing these issues necessitates innovative solutions, such as cost-effective imaging alternatives, Explainable AI frameworks, and comprehensive data-sharing protocols to ensure fairness and transparency.
Regulatory and Ethical Considerations
Navigating the regulatory landscape is critical for the responsible deployment of AI and neuroimaging in mental healthcare. Compliance with data security laws and clinical standards ensures that patient information remains protected amidst growing digital integration. Regulatory bodies are increasingly focused on establishing guidelines that balance innovation with safety, a necessary step for fostering public confidence in these technologies.
Ethical considerations add another layer of complexity, particularly around informed consent and data ownership, as patients must fully understand how their neurological information is used. The risk of over-reliance on technology without clinical judgment also calls for clear policies that prioritize human oversight. Developing robust ethical frameworks is essential to guarantee equitable access and prevent misuse, ensuring that advancements benefit diverse populations without unintended consequences.
The Future of Precision Mental Health
The trajectory of AI and neuroimaging points toward a future where mental healthcare evolves into a highly precise, biology-informed discipline. Near-term advancements are expected to refine diagnostic models, integrating multimodal data for a comprehensive view of brain health. Non-imaging AI tools, such as voice analysis for detecting stress markers, are also gaining traction as complementary methods to traditional scans.
Long-term visions include real-time brain monitoring systems that adapt interventions dynamically, alongside neuromodulation therapies like Transcranial Magnetic Stimulation for targeted treatment. Emerging concepts, such as AI-powered virtual therapists and augmented reality exposure therapy, could bridge access gaps for remote populations. Global economic and regulatory trends will shape these developments, necessitating adaptive strategies to align with varying regional needs and standards.
In reflecting on the insights gathered, it became evident that AI and neuroimaging have opened a new chapter in PTSD diagnosis and care, fundamentally altering how trauma is perceived and managed. The strides made in achieving diagnostic accuracy and personalizing treatments have laid a strong foundation for broader societal acceptance of mental health challenges. Moving forward, stakeholders are encouraged to prioritize the development of ethical guidelines that safeguard patient rights while fostering interdisciplinary collaboration between technologists and clinicians. Investment in accessible, cost-effective solutions is deemed critical to ensure that these innovations reach underserved communities. Ultimately, the journey ahead requires a commitment to balancing technological progress with human-centric values, ensuring that the promise of precision mental health becomes a reality for all.