Listen to the Article
Artificial intelligence (AI) is having a great impact on a large number of industries worldwide—and healthcare is not spared its breadth of innovative capabilities, especially when it comes to bringing a better future to obstetrics. With the growing demand for healthcare to shift from reactive to proactive, personalized treatments, the technology’s power holds significant potential in enhancing both maternal and fetal care outcomes. In fact, in prenatal settings, where timing and early detection are key to avoiding critical and highly vulnerable situations down the road, artificial intelligence offers the tooling necessary to detect complications, pinpoint risks, and monitor development, all done efficiently and at scale.
This article is here to help you take a deeper dive into why artificial intelligence is becoming the go-to source of innovation for maternal healthcare and its impact on imaging, predictive modeling, wearable devices, and genetics—with a focus on why healthcare leaders should prioritize their adoption in 2025 and beyond.
How Does AI-Enhanced Imaging Work in Prenatal Care?
The ultrasound is the most critical tool in the arsenal of prenatal care medical staff. Yet, its utility is more often than not limited to areas that are underserved, rural, or with limited access to comprehensive healthcare. A lack of trained sonographers in such regions makes it challenging to gain an accurate outlook on maternity operations and, until now, there have been few opportunities to bridge this gap and deliver better outcomes. That is, until artificial intelligence took the spotlight, opening a new age of innovation for even less developed communities. Tools like ScanNav FetalCheck are empowering the frontline health workers, regardless of location (and many without specialized radiology training), to perform basic obstetric scans with ease and remarkable accuracy. A pilot research study that took place in Uganda showed the healthcare world the impact of using such a technology-first approach. Antenatal visits that occur earlier during the pregnancy, with high-risk conditions like pre-eclampsia being identified sooner, would have a significant impact on the wellness of both mother and child. And in Malawi, the deployment of AI-supported real-time fetal monitoring during labor was associated with a significant reduction in stillbirths and neonatal deaths.
Additionally, the advantages of artificial intelligence extend well beyond the field of general imaging, expanding into fetal neurosonography, a branch that requires highly specialized interpretation in order to identify neurological anomalies and brain disorders. Through the power of convolutional neural networks, researchers have trained models to identify anomalies such as neural tube defects, hydrocephalus, and congenital heart diseases with sensitivity and accuracy that often exceeds 90%. This switch to high-performing medical models reduces the overall dependence on highly-skilled but limited radiologists and ensures more timely diagnostics, allowing zones where access to advanced neonatal care is limited to standardize healthcare quality and avoid complications that can be avoided through timely interventions.
Another area where artificial intelligence has brought improvements is Fetal Growth Restriction, a major risk factor for perinatal morbidity and mortality. Traditionally, the diagnosis relies on serial growth measurements and Doppler assessments, but both can be highly subjective or, even worse, might be missed entirely.
Artificial intelligence models fully automate the fetal biometry, including head circumference, abdominal diameter, and femur length, an approach that, combined with the Doppler data flows, can deliver marked improvements in the early detection of the disease.
Are Predictive Analytics the Key to Reducing Pregnancy Complications?
There are many complications and disorders that affect the pregnancies of women across the globe. Preterm birth and preeclampsia remain, to this day, two of the most dangerous risks in obstetrics. They often arise suddenly, with limited early symptoms, and achieving successful outcomes depends fully on how fast the medical staff can act, or the tools available.
Artificial intelligence has emerged as a vital solution to changing the tide by shifting detection from reactive to proactive. By aggregating and analyzing essential inputs such as maternal demographics, biomarkers, ultrasound images, and wearable sensor data, AI models can identify at-risk pregnancies and consistently improve their outcomes.
This allows for individualized care plans that enable more intensive observation, device monitoring, prophylactic treatments, or even timely hospitalization when needed, reducing uncertainty and allowing medical staff to act at the best time, with no lost time or resources.
How Does Artificial Intelligence Benefit Wearables and the Practice of Continuous Monitoring?
Sensor technology is a different, more specific part of the healthcare sector that greatly benefits from the emergence and advancement of artificial intelligence—and for a very good reason. Through its heavy usage, pregnancy monitoring can move beyond the clinic’s walls at a much faster rate, bringing a future of next-gen wearable devices that capture electrocardiograms (ECG), uterine contractions, fetal kicks, maternal heart rate, and blood pressure. Algorithms then use this data by processing it to identify early signs of distress. It’s also used to pinpoint abnormal patterns in the pregnancy cycle, which, paired with cloud-based analytics, alerts providers about issues, often before clinical symptoms even appear (all in real-time, with no space left for inaccuracies). The result? A continuous feedback loop, in which both patients and providers are empowered, thus reducing emergency interventions and enhancing confidence in the services offered by healthcare institutions.
Closing Thoughts
As both you and your peers look into the future of maternal and prenatal care and shape the current world for a better future, one thing is clearer than ever: artificial intelligence is no longer a distant possibility or potential factor in innovation—it’s already here, changing how you detect, diagnose and respond to risks during and immediately after pregnancy. From improving access to imaging in underserved communities to using predictive models to flag complications and take action before they can escalate, artificial intelligence is the step forward you need to provide mothers and babies alike with better, safer outcomes. No matter where they live.
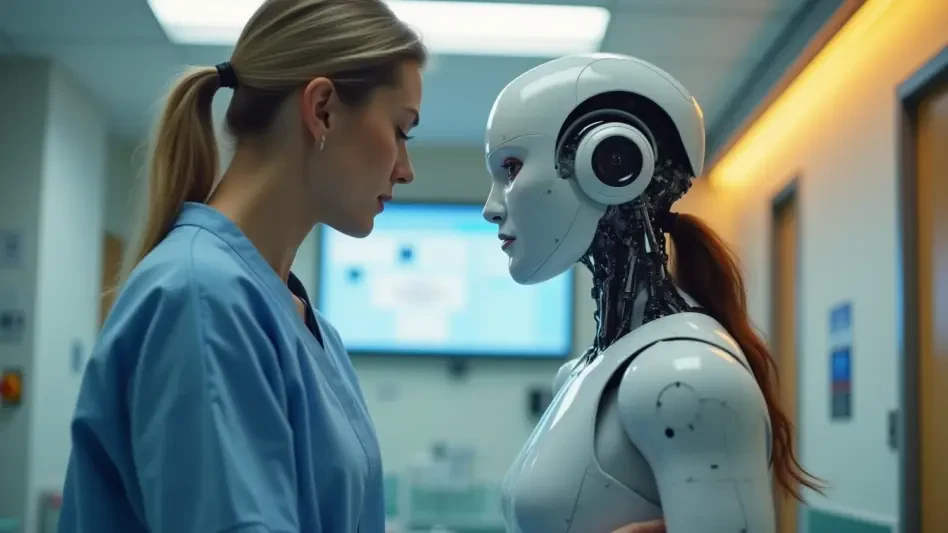
Of course, no technology replaces the importance of skilled care and human connection in medicine. But with the right tools in hand, you have the power to help practitioners spend less time on guesswork and more time where it matters most: with the patient. For healthcare leaders, the message is simple—now is the time to lean into technology, not as a luxury, but as a necessary step toward equity, efficiency, and excellence in maternal health.