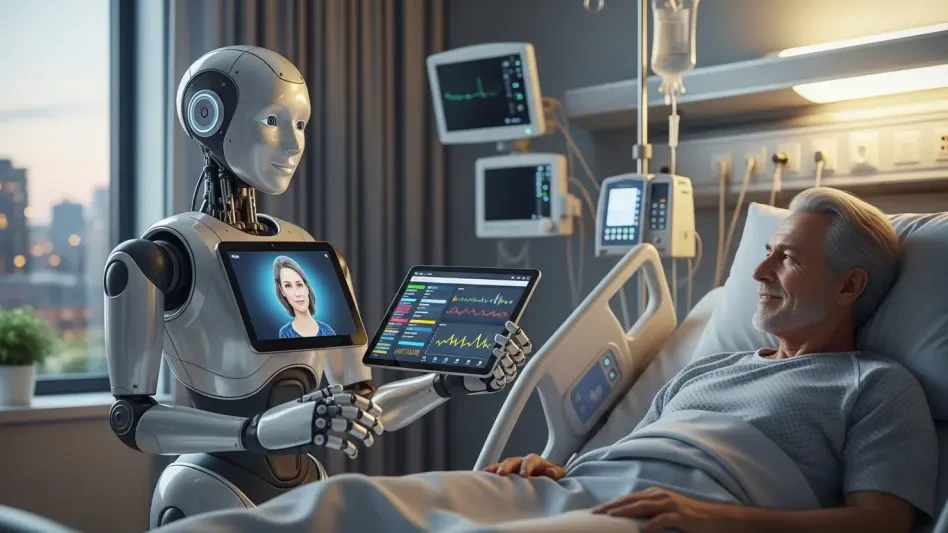
The delicate and often subjective decision of when a patient is ready to be discharged from a hospital has long been a complex variable in healthcare, influenced heavily by a physician’s individual experience and comfort level with risk. This variability can lead to extended hospital stays, which not only strain hospital resources but also expose patients to a higher risk of hospital-acquired infections, falls, and physical deconditioning. Hartford HealthCare sought to address this fundamental challenge by moving beyond subjective assessments and toward a data-driven model. The organization embarked on a mission to standardize and optimize the discharge process by leveraging the power of artificial intelligence to provide objective insights, ultimately aiming to improve patient flow, reduce unnecessary hospital days, and enhance overall patient safety. The goal was not to replace clinical judgment but to augment it with powerful predictive analytics.
A Strategic Fusion of Technology and Clinical Insight
To confront the issue of inconsistent patient discharge timelines, Hartford HealthCare collaborated with an applied mathematician from MIT to co-develop a sophisticated health IT tool known as ##O, or Holistic Hospital Operations. This platform was engineered from the ground up to use artificial intelligence and machine learning algorithms to sift through immense volumes of de-identified patient data. Its primary function is to optimize critical hospital operations, with a specific and impactful focus on enhancing patient flow and throughput. The core challenge was translating raw data into an actionable tool that could genuinely support and empower frontline care teams in their daily decision-making processes. The development process was intentionally inclusive, bringing physician leaders into the design phase to ensure the resulting predictive model was not only statistically accurate but also clinically relevant and aligned with the real-world complexities and challenges faced by medical staff on the hospital floor.
This careful integration of clinical expertise into the technological framework was paramount to the tool’s eventual success. The ##O platform underwent a rigorous pilot phase, where it was tested in a controlled environment and continuously refined based on direct feedback from its end-users: the physicians and care teams. A critical decision for driving adoption was to embed the tool directly into the health system’s existing Epic electronic medical record (EMR) environment. This seamless integration meant that clinicians did not have to log into a separate system or disrupt their established routines. Instead, the AI-powered insights became a natural and accessible part of their daily clinical workflow. By making the technology an unobtrusive yet powerful component of the EMR, Hartford HealthCare effectively lowered the barrier to entry and encouraged consistent use, transforming the ##O tool from a novel concept into a trusted and integral part of patient care management and operational planning.
Redefining Care Coordination with Data-Driven Rounds
The true operational impact of the ##O tool was realized through its incorporation into the health system’s existing daily, multidisciplinary “progression rounds.” These standardized meetings are where care teams convene to review each patient’s case, discuss their progress, and plan the next steps. With the new system in place, these rounds were enhanced with a new, objective data point: the AI-generated discharge readiness prediction. This prediction is now compared directly against the physician-determined expected date of discharge (EDD). When a discordance arises between the AI’s prediction and the physician’s plan, it acts as an immediate trigger for a focused, collaborative discussion. This structured conversation allows the team to proactively identify and address modifiable barriers to a timely discharge—such as pending tests, specialty consults, or post-acute care arrangements—thereby aligning the entire care team and systematically reducing delays that could prolong a patient’s stay unnecessarily.
This synergy between predictive analytics and disciplined operational processes has yielded significant and measurable results across the health system. Within Hartford HealthCare, a predicted discharge readiness assessment is now generated for nearly all admitted medical patients within the first 24 hours of their admission, providing an early and consistent baseline for their care trajectory. The implementation of this integrated approach has led to an approximate 5% reduction in the overall average length of stay when compared to the pre-implementation period. It is emphasized, however, that this achievement was not the result of the AI tool in isolation. Instead, it was the powerful combination of the predictive analytics from ##O, the adherence to disciplined operational workflows like standardized rounds, and improved physician-unit alignment through complementary practices such as geographic rounding that collectively drove this substantial improvement in hospital efficiency and patient care.
A New Precedent for Operational Excellence
The initiative undertaken by Hartford HealthCare established a new benchmark in leveraging advanced analytics to solve longstanding operational hurdles in healthcare. The successful integration of the ##O tool demonstrated that artificial intelligence could serve as a powerful co-pilot for clinicians, augmenting their expertise without undermining their authority. By transforming a subjective process into one supported by objective data, the health system not only improved its patient flow and resource utilization but also fostered a more collaborative and proactive culture among its care teams. This model underscored the critical importance of a holistic approach, proving that technology, when thoughtfully combined with refined clinical processes and strong physician engagement, could produce outcomes far greater than the sum of its parts. The project ultimately provided a clear roadmap for other healthcare organizations looking to harness the power of AI to enhance patient safety and operational efficiency.