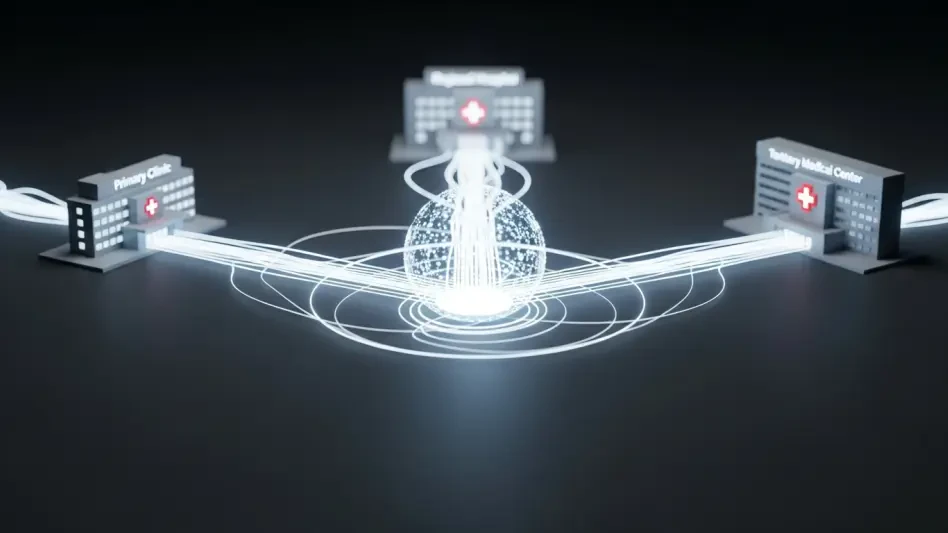
A patient’s medical journey often resembles a fractured narrative, with critical chapters of their health story scattered across unrelated institutions, each holding only a piece of the complete picture. This fundamental disconnect in modern healthcare is more than an inconvenience; it represents a systemic failure where vital information fails to follow the very person it concerns. As patients navigate a complex web of primary clinics, regional hospitals, and specialized tertiary centers, the absence of a unified data-sharing framework introduces significant risks, from redundant and costly procedures to critical delays in diagnosis and treatment. The challenge is not a lack of expertise within these individual facilities, but the absence of a connective tissue that allows them to function cohesively. The question, therefore, is not whether they should cooperate, but whether it is truly possible to architect a system where disparate organizations can operate with the seamlessness of a single, patient-centered entity.
The Siloed State of Modern Healthcare
Navigating a Landscape of Disconnected Care
The modern healthcare landscape is inherently compartmentalized, with patients frequently moving between different levels of care. A journey might begin at a local primary care clinic, escalate to a regional public hospital for intermediate treatment, and culminate at a tertiary medical center for highly specialized procedures. While each institution excels in its designated role, they often operate as independent islands. This structural separation creates what experts call “information discontinuity,” a scenario where a patient’s comprehensive medical history does not travel with them.
This disconnect forces clinicians at each new touchpoint to reconstruct the patient’s story from scratch, relying on incomplete records or the patient’s own recollection. The burden falls not only on the medical staff but also on the patient, who must repeatedly explain their condition, recount past treatments, and navigate a system that lacks a unified memory of their care. This fragmentation undermines the potential for proactive and coordinated treatment, transforming what should be a seamless care continuum into a series of disjointed and often stressful encounters.
The High Cost of Information Fragmentation
The consequences of this informational divide are both clinical and financial. When a specialist at a tertiary hospital lacks immediate access to diagnostic tests performed at a regional facility, those tests are often repeated. This duplication leads to unnecessary costs for the healthcare system and exposes patients to redundant procedures. Moreover, the time spent waiting for records to be transferred or tests to be redone can delay critical care, which is particularly dangerous in time-sensitive cases such as oncology or emergency medicine.
Beyond the direct costs, information fragmentation erodes operational efficiency and compromises patient safety. For regional public hospitals, generating integrated analytics to track population health trends or treatment outcomes becomes an immense challenge without a standardized data flow from partner institutions. From a primary care perspective, monitoring patients referred for specialized treatment becomes a guessing game. Clinicians may struggle to confirm if a patient followed through with an appointment or to receive timely updates on their progress, creating gaps where patients can fall through the cracks of the system.
Pioneering a Unified Care Ecosystem
The Shift Towards Interoperability and Patient-Centric Models
In response to these systemic flaws, a new paradigm is emerging, championed by forward-thinking health networks. The focus is shifting from an institution-centric model, where the hospital is the center of the universe, to a patient-centric one, where the patient’s journey dictates the flow of information. This philosophical shift is powered by a commitment to interoperability—the ability of different information systems and devices to communicate and exchange data seamlessly. At the forefront of this movement is the SMC Best Co-Caring Partners network, a collaborative of diverse institutions committed to breaking down traditional silos.
This network, led by the tertiary Samsung Medical Center (SMC) and including partners like the regional Icheon Medical Center (IMC) and the specialist Samsung Seoul U Surgery Clinic, embarked on a deliberate mission to build a truly integrated ecosystem. Their goal extended beyond simply improving internal processes; they aimed to prove that a multi-organizational collaborative could meet the world’s most rigorous standards for continuity of care. This initiative represents a fundamental re-imagining of healthcare delivery, where technology and process are aligned to serve the patient, regardless of where they receive care.
Quantifying Success with a New Global Benchmark
To validate their pioneering model, the network sought certification under the Healthcare Information and Management Systems Society (HIMSS) Continuity of Care Maturity Model (CCMM). Achieving Stage 6 of this model is not a ceremonial honor; it is an objective, third-party validation that confirms a network’s ability to share and use patient information effectively across different care settings in real-world clinical practice. For the SMC network, this validation was a critical test of their hypothesis that multiple providers can function as a single system.
By becoming the world’s first multi-institution collaborative to earn this distinction, the network has established a new global benchmark. Their success provides a tangible answer to a long-standing industry question, demonstrating that coordinated, digitally enabled care is not just a theoretical concept but an achievable reality. This achievement validates the specific roles of each partner, proving that a regional hospital can be a vital hub and a primary clinic can be a fully integrated starting and ending point for a patient’s care journey.
Bridging the Divide: Overcoming Integration Hurdles
Tackling Technological and Procedural Barriers
The journey toward a unified system was defined by formidable challenges, chief among them the lack of inherent interoperability between the electronic systems of different hospitals. Each institution historically operated with its own set of digital tools and workflows, creating a technological Tower of Babel. Aligning these disparate entities under a single, cohesive framework required a monumental effort in both technology development and process re-engineering. It was not enough to build a bridge; the network had to create a common language and a shared set of traffic rules.
These barriers were not purely technical. Procedural hurdles, such as inconsistent documentation formats and varying timelines for information exchange, had to be systematically dismantled. For a regional public hospital like IMC, another layer of complexity involved generating integrated analytics in collaboration with government agencies, a task complicated by siloed data sources. For a primary care clinic, a key operational challenge was effectively tracking referred patients while respecting their privacy and autonomy—a delicate balance that required new, standardized workflows.
Architecting a Multi-Pronged Solution for Seamless Data Flow
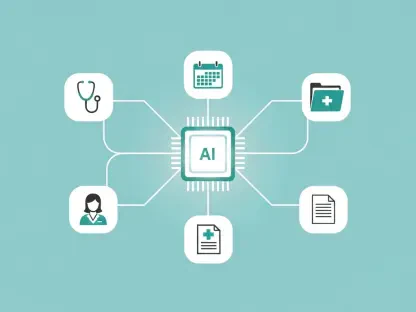
To overcome these obstacles, the network architected a sophisticated, multi-pronged solution. The technological backbone was constructed by integrating Korea’s national Health Information Exchange System with a proprietary Samsung Partners Portal and the Health Insurance Review and Assessment (HIRA) Service. This combination created a standardized digital highway for managing the critical processes of patient referral, return, and follow-up. This core framework was enhanced with optimized image-sharing systems and a dedicated portal to collate data from every phase of a clinical visit.
A key innovation was the direct integration of personal health data from wearable devices, such as smartwatches and continuous glucose monitors, into the Electronic Medical Record (EMR). This allowed clinicians to gain real-time insights into a patient’s daily health status, facilitating more proactive and personalized care. Technology, however, was only one piece of the puzzle. A formal governance structure, coordinated by the SMC Partners Center (SPC), was established to streamline decision-making and ensure alignment on standards. Through iterative joint testing with real patient scenarios, the network refined its processes to guarantee a “closed-loop” flow of accurate and timely information.
The Governance and Standards for Collaborative Health
Building a Foundation of Trust and Standardized Processes
Technology alone cannot foster true collaboration; a foundation of mutual trust and standardized processes is paramount. The network’s success hinged on its ability to cultivate a shared culture of communication and responsibility among clinicians from different institutions. This was achieved through a deliberate and sustained effort to build interpersonal connections and align on clinical best practices. Regular inter-institutional meetings, on-site consulting, and monthly online seminars for doctors became standard practice.
This governance structure ensured that every participant understood their role and responsibilities within the larger ecosystem. For instance, when the validation process revealed inconsistencies in how returned patients were followed up, the network addressed it by expanding the definition of a “closed case” to mandate the completion of a follow-up visit. This seemingly small procedural change had a significant impact, dramatically reducing care fragmentation. While adapting to new documentation standards initially felt burdensome in a busy primary care setting, repeated practice with real patient cases allowed the new workflows to become second nature.
Balancing Patient Privacy with Effective Care Coordination
In any system involving the exchange of sensitive health information, the protection of patient privacy is non-negotiable. The network had to design a framework that balanced the need for effective care coordination with the stringent requirements of data privacy regulations and a patient’s right to choose their provider. This required building robust security protocols into the data exchange platform and establishing clear consent models that gave patients control over their information.
The system was architected to ensure that data was shared on a need-to-know basis, granting clinicians access only to the information relevant to a patient’s current stage of care. The structured referral and return processes also provided a transparent framework for patients, who could see and understand how their information was being communicated between their primary clinic and the hospital. This transparency helped build patient trust, reassuring them that their data was being managed responsibly and for the express purpose of improving their health outcomes.
The Next Frontier in Connected Healthcare
From Manual Exchange to Proactive, Automated Integration
Having achieved a new standard in coordinated care, the SMC network is not resting on its laurels. The next frontier is the transition from a system that requires some manual oversight to one that is fully automated and proactive. The implementation of an API-driven “Proactive Integration Mechanism” is now underway, a system designed to enable real-time, automated data exchange between institutions without human intervention. This will further reduce delays and ensure that a patient’s complete, up-to-the-minute record is available to clinicians at the moment of care.
This technological evolution is about more than just speed; it is about creating a system that can anticipate needs. For example, an automated alert could be triggered if a diabetic patient’s wearable device detects abnormal glucose levels, notifying both their primary care physician and endocrinologist simultaneously. This move toward proactive integration represents a shift from reactive problem-solving to predictive and preventive care, powered by a constant, seamless flow of data across the entire health ecosystem.
Expanding the Ecosystem and Refining Performance Metrics
The future of this model lies in its scalability and continuous refinement. The network plans to expand its partnerships, bringing more healthcare providers into its integrated ecosystem to further enhance the continuity of care across a wider geographical area. As part of this expansion, regional partners like IMC are developing specialized chronic disease management pathways and establishing public health-based data analytics frameworks to better serve their communities.
Simultaneously, the network is refining its key performance indicators (KPIs) to gain deeper insights into the full patient journey. A particular focus is being placed on improving standards for tracking and engaging patients who miss appointments or discontinue treatment, a critical gap in many health systems. By continuously measuring performance and identifying areas for improvement, the network is creating a learning health system—one that not only delivers excellent care today but is also engineered to adapt and improve for tomorrow.
A Proven Blueprint for a Singular Healthcare System
Synthesizing the Tangible Benefits for Patients and Providers
The establishment of this integrated care network yields clear and measurable benefits for all stakeholders. For patients, the experience of care is transformed; they no longer feel like messengers carrying their own fragmented records between appointments. Instead, they are confident that their entire care team is communicating seamlessly, which significantly reduces anxiety and allows them to focus on their health. This coordinated approach leads to fewer redundant tests, shorter wait times, and a clear understanding of their treatment progress.
For providers, the benefits are equally profound. Clinicians gain access to comprehensive patient histories at the point of care, enabling faster and more accurate clinical decision-making. At the primary care level, structured return information from tertiary centers improves the quality of follow-up care, while at the tertiary level, high-quality referral data enhances clinical readiness. This real-time data integration boosts operational efficiency across the network, freeing up valuable resources and allowing medical professionals to practice at the top of their license.
Replicating the Model for a New Era of Coordinated Care
The success of the SMC Best Co-Caring Partners network serves as more than an isolated achievement; it provides a proven, replicable blueprint for health systems worldwide. This model demonstrates that with the right combination of technology, governance, and a shared commitment to patient-centricity, multiple independent healthcare providers can indeed function as a single, integrated ecosystem. It sets a new standard for how a leading tertiary hospital can spearhead a digitally enabled network that empowers regional and primary care partners.
This accomplishment offers a clear path forward for governments and healthcare organizations seeking to overcome the pervasive challenge of information fragmentation. It proves that a regional public hospital can be recognized as a pivotal hub in a connected care network and that primary care clinics can serve as the foundational bedrock of community-based healthcare. The blueprint is now available for others to follow, heralding a new era where coordinated, continuous care is not the exception, but the expected standard for all patients.