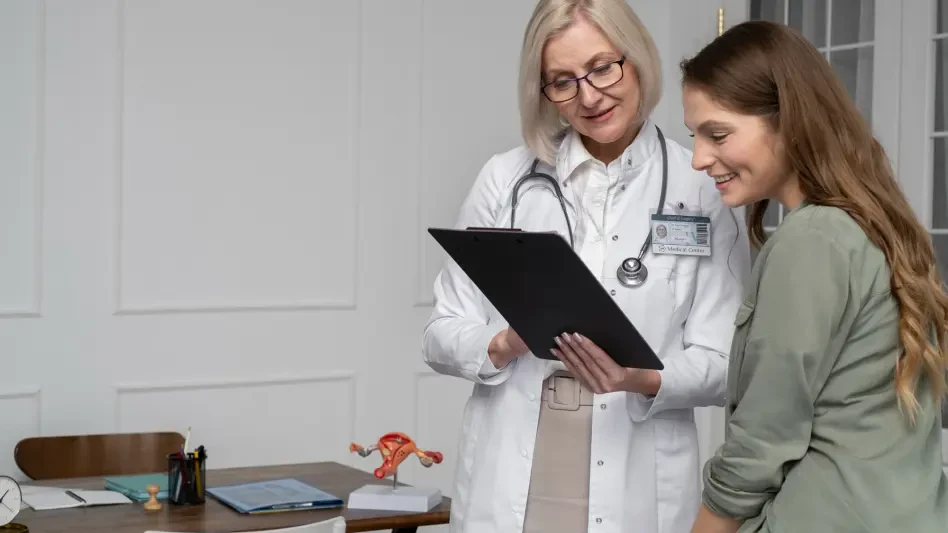
Overview of Women’s Healthcare Challenges in Victoria
In Victoria, Australia, a staggering 90% of women experiencing chronic pain report symptoms lasting over a year, revealing a deep-seated crisis in healthcare equity that demands urgent attention. This alarming statistic underscores a systemic issue where women’s pain is often misunderstood, dismissed, or inadequately treated. The healthcare industry in this region faces mounting pressure to address these disparities, as chronic pain continues to disrupt lives, impacting mental health, employment, and relationships for countless individuals.
The current state of women’s healthcare in Victoria highlights a critical gap in pain management, driven by historical biases and insufficient research tailored to female-specific conditions. Conditions such as endometriosis, menstrual disorders, and musculoskeletal issues disproportionately affect women, yet the medical system has struggled to provide equitable solutions. This challenge has prompted a significant response from policymakers and healthcare leaders, aiming to reshape the landscape of care delivery.
Recent developments have brought these issues into sharp focus, with comprehensive inquiries and reports exposing the extent of the problem. Stakeholders across the sector are now prioritizing reforms to ensure that pain management practices evolve to meet the unique needs of women. This shift marks a pivotal moment for the industry, setting the stage for transformative change in how healthcare is accessed and delivered.
Detailed Analysis of the Gender Pain Gap
Prevalence and Impact of Chronic Pain on Women
Chronic pain imposes a disproportionate burden on women in Victoria, with over half of affected individuals experiencing daily discomfort. Data reveals that 40% of women report pain linked to menstrual or hormonal issues, while 26% cite endometriosis and another 26% point to musculoskeletal disorders as primary sources. These conditions create a persistent barrier to quality of life, often lasting for years without adequate relief.
Beyond physical symptoms, the ripple effects of chronic pain are profound, touching every aspect of daily existence. A staggering 89% of women surveyed indicate significant impacts on mental well-being, with many struggling to maintain employment or nurture personal relationships. This widespread issue calls for urgent attention from healthcare providers to develop targeted interventions that address both the physical and emotional toll.
The industry must recognize that these statistics are not merely numbers but represent real lives disrupted by systemic shortcomings. Addressing this trend requires a shift in how pain is perceived and treated, particularly for conditions historically understudied in women. The data serves as a clarion call for innovation in care models to better support those affected.
Barriers to Accessing Effective Pain Management
Accessing effective pain management remains a formidable challenge for many women, with 68% identifying high costs as a major obstacle. Financial constraints often prevent timely treatment, exacerbating conditions and leading to prolonged suffering. This economic barrier is a critical concern for the healthcare sector, necessitating solutions that prioritize affordability and accessibility.
Equally troubling is the reported dismissal by healthcare providers, with 71% of women feeling their pain is not validated or taken seriously. Such experiences erode trust in the medical system and deter individuals from seeking help. This trend highlights a need for cultural change within the industry to foster empathy and understanding among practitioners.
Intersecting forms of discrimination further compound these challenges, as biases related to race, disability, and weight impact equitable care. Women from diverse communities often face compounded barriers, revealing a complex web of systemic issues. Addressing these disparities demands a multifaceted approach, integrating policy reforms with targeted training for healthcare professionals to ensure inclusive practices.
Systemic Issues and Historical Failures
The healthcare industry in Victoria grapples with entrenched gender bias, where pain management practices have historically failed to account for women’s unique experiences. This oversight has led to dismissive attitudes, leaving many without proper diagnosis or treatment. Such systemic flaws underscore the urgent need for a reevaluation of existing protocols and benchmarks.
Gaps in research on women’s pain exacerbate these challenges, as medical studies have often prioritized male-centric models. This lack of data hinders the development of effective treatments tailored to female physiology, perpetuating cycles of inadequate care. Industry leaders must invest in targeted research to bridge this knowledge gap and inform evidence-based practices.
Unmet health needs, particularly for gynecological and reproductive issues, further illustrate the sector’s shortcomings. Without systemic reform, these issues risk remaining unaddressed, impacting future generations of women. The call for change is clear: the industry must pivot toward comprehensive strategies that prioritize equity and responsiveness to women’s health concerns.
Government Initiatives and Policy Innovations
Transformative Measures for Pain Management
The Victorian Government has taken bold steps to address the gender pain gap by introducing the Women’s Pain Standard, a pioneering framework developed with input from clinicians and affected individuals. This standard seeks to redefine pain management, especially for gynecological procedures like IUD insertions, ensuring women’s experiences are acknowledged and prioritized. Such measures signal a commitment to reshaping industry norms.
Innovative tools like the “green whistle” pain relief are being rolled out as a new benchmark for care, offering immediate relief in clinical settings. Additionally, a specialized clinic at the Royal Children’s Hospital, set to enhance services for adolescents up to age 18, focuses on sexual and reproductive health challenges such as pelvic pain. These initiatives aim to reduce diagnostic delays and improve long-term outcomes for young women.
A broader $153 million women’s health package complements these efforts, encompassing 20 sexual and reproductive health hubs, virtual care options, and dedicated clinics for Aboriginal women. This comprehensive approach reflects a strategic vision to enhance access and quality of care across diverse communities. The industry stands to benefit from these investments as they pave the way for scalable solutions.
Inquiry Recommendations and Action Plans
A recent inquiry into women’s pain has yielded 27 actionable recommendations, forming the backbone of a Women’s Pain Action Plan. This plan sets clear objectives for recognizing and treating pain, addressing systemic barriers, and fostering better understanding among providers. Such structured goals provide a roadmap for sustained progress within the sector.
Key areas of focus include bridging research gaps and tackling biases that hinder equitable care delivery. By prioritizing these recommendations, the government aims to dismantle longstanding inequities and build a more responsive healthcare system. Collaboration between policymakers and industry stakeholders will be essential to translate these goals into tangible outcomes.
The emphasis on diverse community needs within the action plan ensures that reforms are inclusive, addressing intersectional challenges faced by marginalized groups. As these policies unfold over the coming years, from now through 2027, their impact on care access and quality will be closely monitored. This forward-thinking approach positions Victoria as a leader in healthcare equity.
Future Trends in Women’s Pain Management
Growing Recognition and Advocacy
The gender pain gap is increasingly acknowledged as a critical public health issue, with Victorian leaders uniting in a call for systemic change. This growing awareness is driving momentum for reform, as advocacy groups and policymakers collaborate to elevate women’s voices. The trend signals a cultural shift within the industry toward greater accountability and empathy.
Community advocacy plays a pivotal role in sustaining this momentum, ensuring that the needs of affected individuals remain at the forefront of policy discussions. Grassroots movements are pushing for continued investment in research and training, amplifying the demand for equitable practices. This collective effort is reshaping the narrative around pain management.
Global trends in women’s health also inform local strategies, as Victoria aligns with international calls for gender-specific healthcare research. By learning from broader advancements, the region can adopt best practices tailored to its unique context. This alignment promises to enhance the effectiveness of ongoing and future reforms.
Evolving Research and Healthcare Practices
Advancements in research are poised to transform how women’s pain is understood and treated, with a focus on filling historical data gaps. Industry investment in studies specific to female physiology will likely yield new insights, enabling the development of targeted therapies. This shift is essential for addressing long-standing disparities in care.
Healthcare practices are also evolving, with an emphasis on training providers to recognize and mitigate gender bias. Programs aimed at fostering cultural competence are gaining traction, equipping professionals with tools to deliver personalized care. Such initiatives are critical for rebuilding trust among patients who have felt dismissed.
The integration of technology, such as virtual care platforms, offers additional avenues for improving access to pain management. These innovations can bridge geographic and economic barriers, ensuring more women receive timely support. As these practices mature, they will likely redefine standards of care across the sector.
Reflecting on Findings and Next Steps
Looking back, the comprehensive inquiry into women’s pain in Victoria exposed critical disparities that had long been overlooked, marking a turning point for the healthcare industry. The detailed findings painted a sobering picture of systemic bias and unmet needs, while highlighting the profound impact of chronic pain on women’s lives. Government responses, including new standards and specialized clinics, demonstrated a commitment to change that resonated across the sector.
Moving forward, the focus must shift to sustained implementation of the inquiry’s recommendations, ensuring that policies translate into measurable improvements. Stakeholders should prioritize partnerships between research institutions and healthcare providers to drive innovation in pain management. Establishing regular evaluations of progress, particularly in addressing intersectional barriers, will be crucial for maintaining accountability.
Additionally, empowering communities through education and advocacy emerged as a vital next step, ensuring that women continue to have a platform to share their experiences. By fostering an environment where pain is validated and treated with urgency, Victoria sets a precedent for other regions to follow. The journey toward equity in healthcare demands ongoing vigilance and adaptability to meet evolving needs.