The life-saving biologic drug in a hospital patient’s IV drip likely began its journey years ago in a single, colossal factory thousands of miles away, a fact that represents both a triumph of modern science and a critical vulnerability. For decades, the biopharmaceutical industry has relied on this “bigger is better” philosophy, constructing immense, centralized manufacturing plants to produce blockbuster drugs at a global scale. This model, built on the premise of a stable and predictable world, is now showing signs of strain under the weight of modern pressures. The very foundation of how advanced medicines are made is being challenged by a confluence of geopolitical instability, persistent supply chain disruptions, and a fundamental shift in the nature of therapeutic innovation itself, forcing the industry to question whether the age of the mega-factory is drawing to a close.
The Blockbuster Hangover and Its Consequences
The mega-factory model was a creature of the blockbuster era, a time when a handful of high-volume drugs dominated the market and justified the massive capital investment. These facilities, often costing upwards of $200 million and taking three to five years to construct, were engineered for one primary purpose: high-throughput production of a single product. This singular focus, once a symbol of efficiency, has become a significant liability in an industry that is rapidly moving away from one-size-fits-all solutions. The model created an inherent rigidity, locking companies into specific product lines and making it difficult to pivot in response to evolving patient needs or new therapeutic discoveries.
This inflexibility has tangible consequences for patients. The reliance on a few large, globally dependent sites creates bottlenecks that ripple across the entire supply chain. When a single facility faces delays due to shortages of raw materials, equipment, or outsourced components, critical clinical and commercial programs can grind to a halt. This fragility is a contributing factor to long-standing drug shortages, which in the United States now last for an average of over four years. The blockbuster hangover is not merely an operational headache for manufacturers; it is a direct threat to patient access to essential medicines, exposing the systemic risk embedded in a manufacturing strategy that prized scale above all else.
Cracks in the Foundation of Centralized Manufacturing
The forces dismantling the old model are both external and internal. Geopolitical instability and ongoing supply chain crises have shattered the illusion of a frictionless global economy, revealing the precariousness of relying on a single point of production. However, an equally powerful catalyst for change is coming from within the industry’s own research and development pipelines. The world of biopharma is no longer defined solely by blockbusters. Instead, it is becoming increasingly fragmented and precise, with a focus on personalized medicine and targeted therapies for smaller patient populations.
Over the past decade and a half, the number of protein-based therapies entering Phase 1 clinical trials has doubled, a testament to the pace of innovation. Critically, an estimated 50% of new biologics are now classified as rare or orphan drugs, designed to treat conditions affecting far fewer people than the ailments targeted by traditional blockbusters. This shift demands a manufacturing paradigm that is just as precise and targeted as the medicines themselves. The mega-factory, with its vast stainless-steel bioreactors built for massive volumes, is fundamentally ill-equipped to handle the demand for small-batch, flexible production that defines the future of medicine.
A New Blueprint for an Agile and Distributed Future
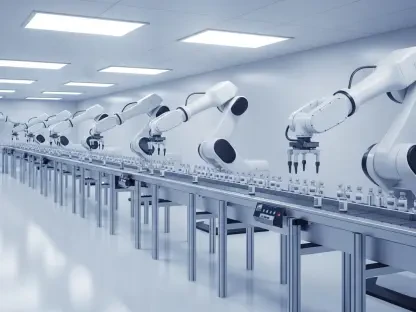
In response to these challenges, a new manufacturing blueprint is emerging, one built not on monolithic scale but on agility, technology, and distribution. This modern approach is enabled by significant advancements in bioprocessing, particularly the adoption of intensified, continuous, and modular systems. These innovations are making decentralized production networks not only operationally advantageous but also economically viable. The new model replaces cavernous production halls with compact, efficient, and highly automated systems that can be deployed regionally, closer to the patients who need them.
Continuous manufacturing stands at the forefront of this technological revolution. By moving away from traditional, stop-and-start batch processes, this approach can reduce the required equipment footprint by as much as 70% while simultaneously increasing volumetric productivity by a factor of three to five. The benefits extend beyond efficiency; continuous processes often lead to higher product quality and consistency. Coupled with modular, closed, and automated systems, this technology allows smaller, regional facilities to operate with remarkable precision and reduced staffing needs. Consequently, this lowers overall facility costs by 30–50%, democratizing access to high-quality biomanufacturing capabilities.
Forging a New Path with Next Generation Facilities
This transition is not merely theoretical; it is already being put into practice by forward-thinking companies and supported by global regulators. A crucial enabler has been the growing regulatory acceptance of these novel technologies. Authorities are increasingly approving modular, single-use, and continuous production systems for both clinical and commercial supply, signaling a clear path forward for the industry. This regulatory green light has paved the way for pioneering companies to build the next generation of biomanufacturing facilities.
Real-world examples illustrate the viability of this new model. In Ireland, WuXi Biologics received approval from the European Medicines Agency for a commercial manufacturing site that utilizes one of the world’s largest cell culture processes based on single-use, continuous technology. In the United States, Enzene Biosciences inaugurated a facility in New Jersey deploying the first fully-connected continuous manufacturing platform validated for commercial biologics, enabling a “copy-exact” model that allows for the seamless transfer of a process from its R&D center in India. Meanwhile, BiosanaPharma achieved a major milestone by producing the first monoclonal antibody manufactured with a fully continuous process to enter clinical trials. These successes demonstrate that an agile, distributed network is no longer a future concept but a present-day reality.
The biomanufacturing industry found itself at a definitive turning point. The combined pressures of a changing therapeutic pipeline, persistent global instability, and profound technological innovation compelled a strategic evolution away from complete reliance on the mega-factory. The future was defined by a hybrid network, one that strategically integrated large, centralized plants for high-volume products with a constellation of smaller, more flexible regional sites. This new model proved essential for enhancing resilience, mitigating supply chain risks, and, most importantly, accelerating patient access to an increasingly diverse portfolio of life-saving therapies. For this vision to be fully realized, a robust partnership between regulators and manufacturers was needed to establish clear quality risk management standards for distributed manufacturing, a collaboration that became vital to ensuring the safety and efficacy of biologics produced across the decentralized network.