Rural health care stands at a critical juncture, grappling with systemic challenges while serving a significant portion of the American population, with rural hospitals catering to 25% of the nation’s citizens and comprising 35% of all U.S. hospitals. The stakes for innovation and transformation are extraordinarily high in these facilities, which often operate in geographically isolated areas, facing barriers to access, funding shortages, and workforce limitations that threaten their sustainability. Yet, amidst these struggles lies an opportunity to redefine health care delivery through cutting-edge solutions and collaborative efforts. This report delves into the current state of rural health care, explores emerging trends, tackles persistent challenges, and envisions a future where innovation bridges longstanding gaps.
Understanding the Current Landscape of Rural Health Care
Rural health care plays an indispensable role in the American health care ecosystem, ensuring that millions of individuals in remote areas receive essential medical services. Despite its significance, the sector faces daunting obstacles, including limited access to specialized care due to vast distances and a scarcity of local providers. Many rural hospitals struggle to maintain financial viability, with closures becoming a recurring concern as operational costs outpace revenue in sparsely populated regions.
The challenges are compounded by systemic issues such as inadequate funding and difficulties in recruiting and retaining medical professionals willing to work in isolated settings. Geographic isolation not only hampers patient access but also complicates the delivery of emergency services, often resulting in delayed care. These barriers highlight the urgent need for transformative approaches to sustain rural health systems.
Key stakeholders shaping this landscape include hospital leaders who manage day-to-day operations, policymakers crafting legislative solutions, and technology innovators developing tools to overcome logistical hurdles. Medical associations like the American Hospital Association (AHA) and the American Medical Association (AMA) also play a pivotal role by advocating for policies and resources to bolster rural facilities. Together, these groups form a coalition dedicated to addressing the unique needs of rural communities through strategic interventions.
Emerging Trends and Opportunities in Rural Health Care
Key Innovations Driving Change
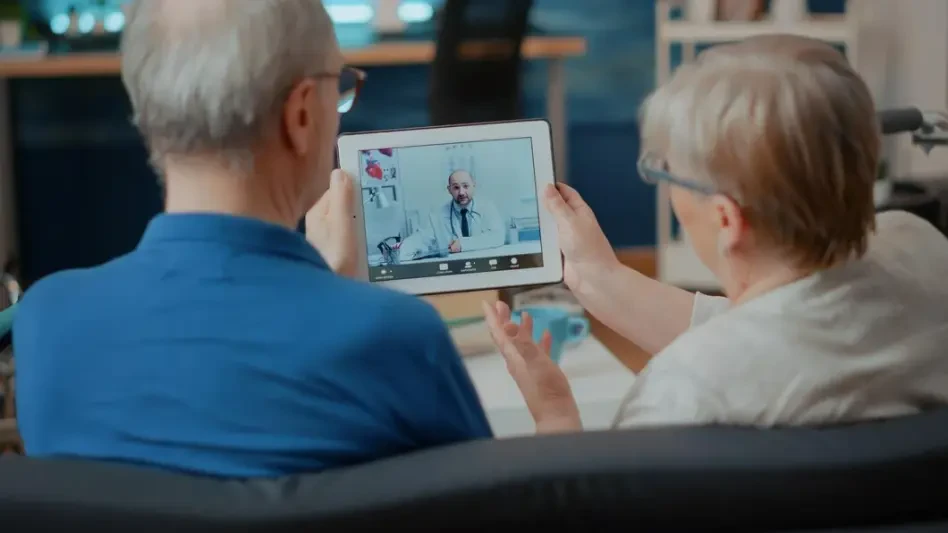
Technological advancements are paving the way for significant improvements in rural health care delivery, addressing long-standing resource constraints. Artificial intelligence (AI) and data analytics are being harnessed to optimize operations, predict patient needs, and enhance diagnostic accuracy, even in understaffed facilities. Telehealth, in particular, has emerged as a game-changer, enabling remote consultations and reducing the burden of travel for patients in far-flung areas.
Beyond technology, innovative care models are gaining traction as rural providers adapt to evolving demands. Provider-aligned plans, which integrate care delivery with financial incentives for health outcomes, are fostering more coordinated and efficient systems. Additionally, patient-centered approaches prioritize individual needs, ensuring that treatments align with the cultural and personal contexts of rural populations.
A parallel trend involves cultural transformation within rural health care settings, emphasizing trust-building with local communities. By engaging residents in decision-making processes and showcasing the dedication of caregivers, hospitals can strengthen public support. This shift toward community involvement is proving essential for sustaining long-term improvements and fostering resilience in rural health systems.
Market Insights and Growth Potential
Data-driven insights reveal a promising horizon for rural health care, with substantial investments on the table to drive change. A proposed $50 billion Rural Health Transformation Program aims to inject critical funding into innovative projects, with the potential to redefine care delivery over the next several years. Such initiatives underscore a growing recognition of rural health as a national priority with ripple effects beyond local boundaries.
Growth projections indicate a rapid uptake of technology in rural settings, with telehealth and AI adoption expected to expand significantly from now through 2027. Industry leaders anticipate that these tools will not only improve access and affordability but also serve as models for urban health care systems facing similar pressures. The scalability of rural solutions holds promise for broader application, potentially transforming how care is delivered nationwide.
Expert perspectives further illuminate the path forward, with many emphasizing the need for tailored solutions that address specific rural challenges. Hospital executives and technology pioneers alike stress that investments must prioritize infrastructure to support digital tools while ensuring equitable distribution of benefits. This dual focus on innovation and fairness is seen as key to unlocking the full potential of rural health care advancements.
Challenges Facing Rural Health Care Transformation
The journey toward transforming rural health care is fraught with obstacles that demand creative and collaborative responses. Limited funding remains a primary barrier, as many rural hospitals operate on thin margins, unable to invest in new technologies or expand services. This financial strain is often exacerbated by declining populations in rural areas, which reduce patient volumes and further stress revenue streams.
Workforce shortages pose another significant hurdle, with rural facilities struggling to attract physicians, nurses, and specialists. The lack of local training opportunities and the allure of urban career prospects deter professionals from committing to remote postings. Additionally, gaps in technological infrastructure, such as unreliable internet connectivity, hinder the adoption of digital health solutions that could otherwise alleviate some of these pressures.
To address these issues, public-private partnerships offer a viable strategy by pooling resources and expertise to fund critical projects. Community engagement initiatives can also play a role by fostering local support and advocacy for health care improvements. Moreover, pushing for policy reforms to tackle systemic inequities—such as increased reimbursement rates for rural providers—could provide a much-needed lifeline to struggling facilities.
Navigating the Regulatory and Policy Environment
The regulatory framework surrounding rural health care significantly influences the pace and direction of innovation. Federal and state funding initiatives are being proposed to bolster rural hospitals, with programs aimed at enhancing infrastructure and supporting technology integration. These investments are critical for ensuring that rural providers can keep up with the demands of modern health care delivery.
Compliance remains a complex issue, particularly as new technologies like AI are introduced into clinical settings. Regulatory bodies must balance the need for oversight with the urgency of innovation, ensuring that safety and efficacy standards are met without stifling progress. Policymakers are increasingly tasked with crafting guidelines that facilitate the responsible deployment of such tools in resource-limited environments.
Insights from Centers for Medicare & Medicaid Services (CMS) leaders and other officials highlight the importance of equity in policy design. Ensuring that rural communities receive fair access to funding and technological advancements is a recurring theme in discussions. This focus on equitable distribution is essential for building a health care system that serves all Americans, regardless of geographic location.
The Future of Rural Health Care: Vision and Disruptors
Looking ahead, the trajectory of rural health care is poised to be shaped by groundbreaking technologies and evolving societal dynamics. Advanced telehealth platforms are expected to further bridge the gap between patients and providers, offering seamless access to specialized care. Predictive analytics, meanwhile, could enable proactive interventions by identifying health risks before they escalate into crises.
Potential disruptors, such as shifting demographics and economic fluctuations, may introduce new challenges to rural health systems. Aging populations in many rural areas could strain existing resources, while economic downturns might limit funding for health initiatives. Staying ahead of these factors will require adaptive strategies and a willingness to rethink traditional care delivery models.
Consumer preferences are also driving change, with a growing demand for accessible and affordable health care options. Collaboration among stakeholders—hospitals, tech firms, and policymakers—will be crucial for meeting these expectations and ensuring sustainable growth. Drawing on the optimism expressed at industry summits, the future of rural health care hinges on actionable plans that prioritize innovation while addressing the unique needs of rural communities.
Conclusion: A Roadmap for Transformative Change
Reflecting on the discussions held at pivotal industry gatherings like the Sioux Falls Summit, it became evident that rural health care has reached a turning point demanding urgent action. The event underscored the vital role of advocacy, technology, and policy reform in reshaping the sector for better outcomes. Key challenges such as funding shortages and access barriers were thoroughly examined, revealing both the complexity of the issues and the potential for impactful solutions.
Moving forward, stakeholders were encouraged to prioritize investments in scalable innovations, particularly in telehealth and data-driven tools that could enhance care delivery. Amplifying community narratives emerged as a powerful strategy to build trust and influence legislative agendas, ensuring that rural voices are heard at national levels. By fostering cross-sector collaboration, the groundwork was laid for a more equitable health care system.
The path ahead calls for a sustained commitment to patient-centered solutions, with an emphasis on tailoring interventions to the specific cultural and geographic contexts of rural areas. Recommendations included establishing more robust public-private partnerships to fund infrastructure upgrades and advocating for policies that address systemic disparities. These steps, rooted in the collective resolve witnessed at industry forums, offer a blueprint for achieving lasting transformation in rural health care.