Imagine a world where a patient, feeling unwell at midnight, can instantly consult a virtual assistant that not only understands their symptoms but also schedules a doctor’s appointment or suggests immediate care options—all without leaving the comfort of home. This scenario is no longer a distant dream but a tangible reality powered by artificial intelligence (AI) in healthcare. The integration of AI is transforming the way patients interact with medical systems, redefining access, engagement, and care delivery. This review dives deep into the technological advancements driving this shift, evaluates their performance, and explores the profound impact on the healthcare landscape, shedding light on both the promise and the challenges of this digital revolution.
The Rise of AI as Healthcare’s Digital Front Door
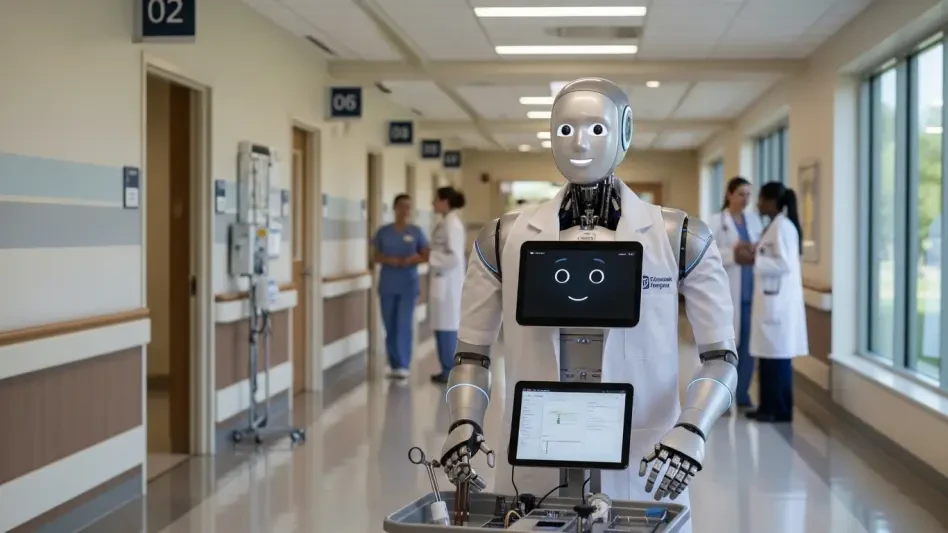
AI has emerged as a pivotal force in reshaping the initial point of contact between patients and healthcare providers, often termed the “digital front door.” This concept encompasses a suite of tools like virtual assistants, symptom checkers, and personalized health portals that provide round-the-clock access to medical guidance. The technology addresses a critical need for efficiency in an overburdened system, where long wait times and administrative hurdles often deter timely care. By leveraging AI, healthcare organizations aim to streamline these interactions, making them more accessible and user-friendly for patients across diverse demographics.
The significance of this transformation lies in its ability to empower individuals with unprecedented control over their health decisions. Patients can now assess minor ailments, book consultations, or manage chronic conditions through intuitive digital interfaces. This shift aligns with broader consumer expectations for on-demand services, mirroring trends seen in other industries like retail and finance. However, the adoption of such tools also raises questions about trust, accuracy, and the preservation of human connection in medical care, setting the stage for a detailed examination of AI’s capabilities and limitations.
Core Technologies Driving AI in Healthcare
Natural Language Processing and Conversational AI
At the heart of AI’s interaction with patients is Natural Language Processing (NLP), a technology that enables machines to understand and respond to human language with remarkable precision. Advanced transformer models like BERT and GPT power conversational AI, allowing virtual assistants to interpret complex patient inquiries, whether typed or spoken. This capability ensures that a user describing vague symptoms receives relevant prompts or advice, mimicking the nuance of human dialogue and enhancing engagement.
The performance of conversational AI has seen significant strides, with systems now achieving high accuracy in understanding context and intent. These tools are integral to virtual health assistants deployed by hospitals and clinics, where they handle tasks like triaging symptoms or guiding patients through administrative processes. Beyond functionality, NLP fosters a seamless communication experience, reducing frustration and building confidence in digital healthcare platforms.
A key strength of this technology is its adaptability to diverse linguistic patterns and dialects, making it accessible to a broader audience. However, challenges remain in handling highly specialized medical jargon or emotional nuances that require empathetic responses. Continuous refinement of these models is essential to ensure they meet the intricate demands of patient interaction without misinterpretation.
Machine Learning and Predictive Analytics
Machine Learning (ML) forms another cornerstone of AI in healthcare, excelling in the analysis of vast datasets to deliver personalized care and actionable insights. By processing historical health records, ML algorithms can identify patterns, such as predicting which patients are at risk of developing chronic conditions like diabetes. This predictive power enables proactive interventions, potentially saving lives and reducing long-term costs for healthcare systems.
Beyond individual care, ML optimizes operational aspects like appointment scheduling by forecasting demand and minimizing wait times. Performance metrics indicate that ML-driven tools often outperform traditional methods, with error rates in risk prediction dropping significantly in recent implementations. Such efficiency not only improves patient satisfaction but also alleviates administrative burdens on medical staff, allowing them to focus on direct care.
Despite these advantages, the technology’s effectiveness hinges on the quality and diversity of data it processes. Incomplete or biased datasets can skew predictions, leading to disparities in care delivery. Addressing these gaps through robust data collection and validation protocols remains a critical area for improvement to maximize ML’s impact on healthcare outcomes.
Data Integration and Interoperability
The fragmented nature of healthcare data poses a significant barrier to cohesive patient care, a challenge AI tackles through advanced data integration and interoperability. Technologies like Knowledge Graphs organize disparate information into structured, accessible formats, while standards such as HL7 FHIR ensure seamless data exchange across systems. This integration creates unified patient records, enabling providers to make informed decisions based on comprehensive health histories.
Interoperability is particularly vital in enhancing the digital experience, as it allows various platforms—whether hospital databases or patient apps—to communicate effectively. For instance, a symptom checker can pull real-time data from electronic health records to offer tailored recommendations. The result is a smoother journey for patients navigating complex medical systems, with fewer delays or errors due to missing information.
Nevertheless, achieving full interoperability faces hurdles, including inconsistent adoption of standards and concerns over data security during transfers. Strengthening compliance with protocols and investing in secure infrastructure are necessary steps to ensure that AI-driven integration fulfills its promise of transforming fragmented data into a cohesive, actionable resource.
Recent Innovations and Market Trends
The landscape of AI in healthcare continues to evolve rapidly, with recent advancements pushing the boundaries of what digital tools can achieve. Chatbot functionality has improved, moving beyond basic responses to managing intricate patient journeys, such as guiding users through pre-diagnosis steps or follow-up care plans. These enhancements reflect a growing sophistication in AI’s ability to handle nuanced interactions, meeting rising consumer demand for personalized, immediate healthcare services.
Another notable trend is the emergence of multimodal AI, which integrates diverse data sources like text, images, and sensor inputs to provide holistic insights. For example, combining wearable device data with patient-reported symptoms can lead to more accurate assessments. Additionally, generative AI is gaining traction, with applications in creating tailored health education content or simulating medical scenarios for training, pointing to a dynamic shift in how technology supports both patients and providers.
Consumer expectations are also shaping market dynamics, with a clear preference for on-demand, patient-centric models over traditional, rigid systems. This demand drives investment in AI solutions, with the global market projected to grow substantially from now to 2027. As stakeholders prioritize user experience and clinical validation, the focus remains on balancing innovation with reliability to maintain trust in these transformative tools.
Real-World Implementations and Impact
AI’s practical applications in healthcare settings demonstrate its capacity to revolutionize care delivery across various contexts. Virtual symptom checkers, for instance, are widely deployed in hospitals and clinics, enabling patients to input symptoms and receive preliminary guidance on whether to seek urgent care. Companies like Ada Health have pioneered such tools, offering accessible solutions that cater to millions globally, often in multiple languages to broaden reach.
Appointment scheduling tools powered by AI further illustrate the technology’s value, automating a process that once consumed significant staff time. Health management portals, integrated into major systems by tech giants like Google and Microsoft, allow patients to track conditions, view test results, and communicate with providers through a single interface. These implementations enhance efficiency, reducing no-show rates and improving overall access to services.
A particularly impactful use case is AI’s deployment in underserved regions, where access to medical professionals is limited. Digital platforms bridge this gap by providing basic diagnostic support and connecting remote patients to telehealth services. Such initiatives highlight AI’s potential to democratize healthcare, though they also underscore the need for infrastructure support to ensure equitable benefits across populations.
Challenges Hindering AI Adoption
Despite its promise, AI in healthcare faces several obstacles that temper its widespread adoption. Technical challenges, such as algorithmic bias, pose a risk of perpetuating disparities if models are trained on unrepresentative data. For example, biased algorithms might underdiagnose certain conditions in minority groups, undermining trust and effectiveness in diverse communities.
Regulatory hurdles also loom large, particularly around data privacy and compliance with laws governing health information. The sensitive nature of medical data demands stringent security measures, yet breaches remain a concern as systems scale. Market barriers, including the digital divide, further complicate deployment, as not all patients have access to the necessary technology or digital literacy to engage with AI tools, exacerbating existing inequities.
Efforts to address these issues are underway, with bias audits gaining traction to identify and correct skewed algorithms. Robust encryption and privacy frameworks are being developed to safeguard data, while infrastructure investments aim to close access gaps in rural or low-income areas. Overcoming these challenges requires a collaborative approach among technologists, policymakers, and healthcare leaders to ensure AI serves as an inclusive, trustworthy solution.
Looking Ahead: The Future of AI in Healthcare
The trajectory of AI in healthcare points to both near-term refinements and ambitious long-term visions. Over the next few years, expect enhancements in digital tools like chatbots, which will manage more complex interactions, such as coordinating multi-step care plans. These incremental improvements aim to bolster user confidence by delivering consistent, accurate support tailored to individual needs.
In the longer horizon, the concept of personalized AI health assistants for every individual emerges as a transformative goal. Such assistants could monitor health continuously, predict potential issues, and recommend preventive measures, fundamentally shifting care from reactive to proactive. Multimodal AI, integrating varied data streams, promises to elevate diagnostic precision, potentially identifying conditions before symptoms manifest.
The societal impact of these advancements could be profound, reshaping how healthcare is perceived and accessed. However, realizing this future demands addressing persistent issues like trust, data quality, and equitable access. Regulatory clarity and ethical guidelines will play a pivotal role in ensuring that AI evolves as a force for good, balancing technological progress with the core values of compassionate, patient-centered care.
Final Reflections
Looking back, this review illuminated how AI redefined healthcare through innovative tools that enhanced patient access and streamlined operations. The journey revealed the power of technologies like NLP, machine learning, and data integration in creating a digital front door that empowered individuals while easing burdens on providers. Challenges such as bias, privacy risks, and access disparities stood out as critical hurdles that demanded attention.
Moving forward, stakeholders must prioritize actionable solutions like bias mitigation strategies, stronger data security protocols, and targeted investments in underserved communities to bridge the digital divide. Collaboration across sectors should focus on building transparent, reliable systems that patients and providers alike can trust. As the field advances, integrating human empathy with technological efficiency remains paramount, ensuring that AI amplifies rather than diminishes the heart of healthcare.